Pediatric Fractures and Dislocations
"Learn about the general principles of pediatric orthopaedic surgery, including epidemiology, anatomy, mechanism of injury, clinical evaluation, radiographic evaluation, classification, treatment, and complications."
OVERVIEW
The development and growth of the skeletal system from gestation to skeletal maturity create interrelated fibrous, tendinous, cartilaginous, and osseous changes resulting in patterns of susceptibility and reparative response that distinguish the pediatric patient from the adult.
As a rule, the younger the patient, the greater the remodeling potential; thus, absolute anatomic reduction in a child is less important than in a comparable injury in an adult.
EPIDEMIOLOGY
- The incidence of pediatric fractures is increasing.
- The increasing fracture incidence in children has been mainly attributed to increased sports participation.
- Approximately 50% of all children will fracture at least one bone during childhood.
- The overall mortality rate of children has fallen from 1 in 250 per year in 1900 to 1 in 4,000 per year in 1986; this has been attributed to improved public education, preventive devices, and medical care.
- The leading cause of death in children ages 1 to 14 years is accidental trauma.
- Skeletal trauma accounts for 10% to 15% of all childhood injuries, with approximately 15% to 30% of these representing physeal injuries (phalanx fractures are the most common physeal injury).
- From the ages of 0 to 16 years, 42% of boys will sustain at least one fracture compared with 27% of girls.
- The overall ratio of boys to girls who sustain a single, isolated fracture is 2.7:1. The peak incidence of fractures in boys occurs at age 16 years, with an incidence of 450 per 10,000 per year; the peak incidence in girls occurs at age 12 years, with an incidence of 250 per 10,000 per year.
- Open fractures in this population are rare (<5%).
ANATOMY
Pediatric bone has a higher water content and lower mineral content per unit volume than adult bone. Therefore, pediatric bone has a lower modulus of elasticity (less brittle) and a higher ultimate strain-to-failure than adult bone. It is relatively stronger in tension than compression, as compared to adult bone.
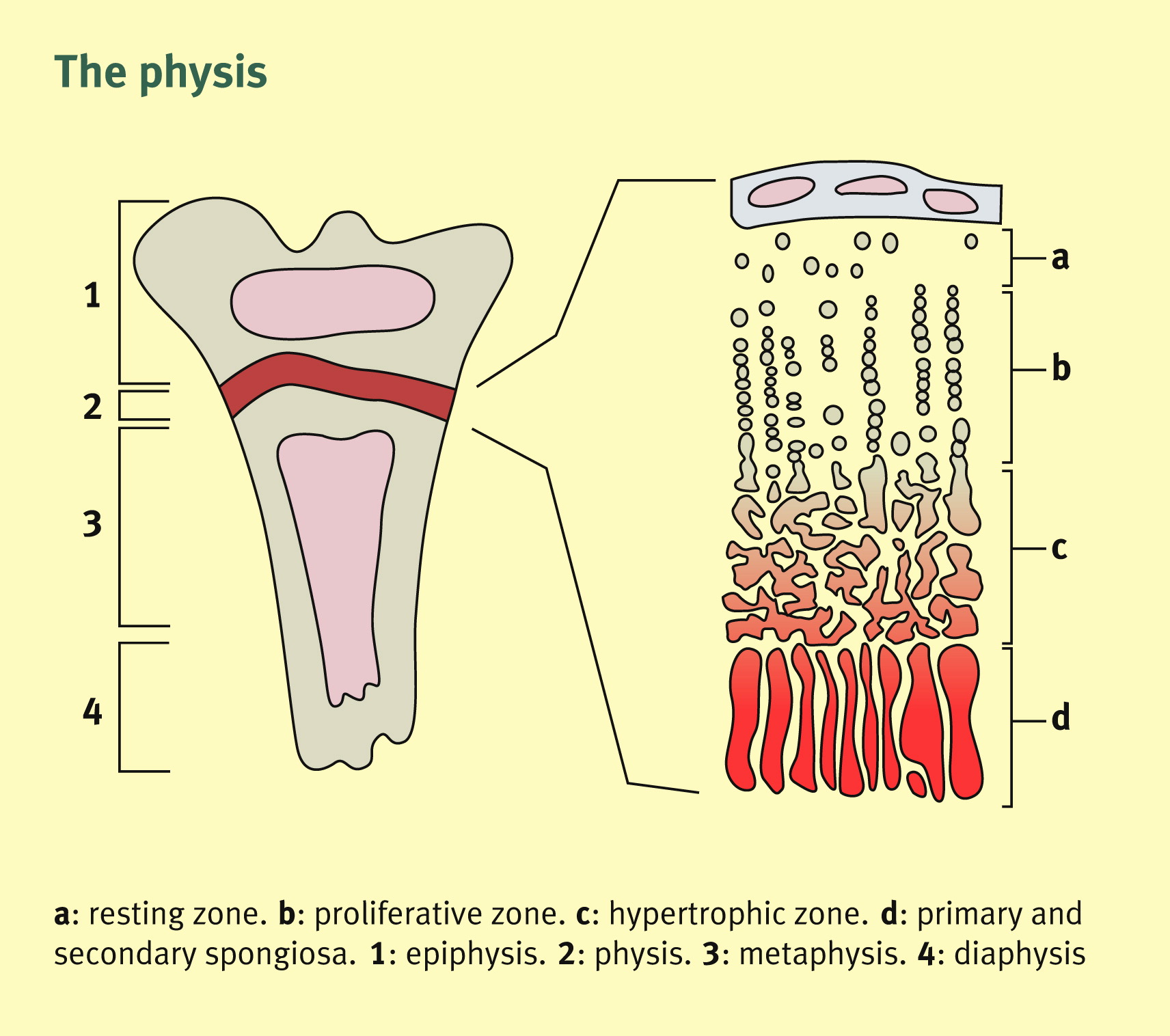
The physis (growth plate) is a unique cartilaginous structure that varies in thickness depending on age and location. It is frequently weaker than bone in torsion, shear, and bending, predisposing the child to injury through this delicate area.
The physis is traditionally divided into four zones: reserve (resting/germinal), proliferative, hypertrophic, and provisional calcification (or enchondral ossification) (Fig. 42.1).
The periosteum in a child is a thick fibrous structure (up to several millimeters) that encompasses the entire bone except the articular ends. The periosteum thickens and is continuous with the physis at the perichondral ring (ring of LaCroix), offering additional resistance to shear force.
As a general rule, ligaments in children are functionally stronger than the physis. Therefore, a higher proportion of injuries that produce sprains in adults result in physeal fractures in children.
The blood supply to the growing bone includes a rich metaphyseal circulation with fine capillary loops ending at the physis (in the neonate, small vessels may traverse the physis, ending in the epiphysis).
MECHANISM OF INJURY
Because of structural differences, pediatric fractures tend to occur at lower energy than adult fractures. Most are a result of compression, torsion, or bending moments.
Compression fractures are found most commonly at the metaphyseal diaphyseal junction and are referred to as “buckle fractures” or “torus fractures.” Torus fractures rarely cause physeal injury, but they may result in acute angular deformity. Because torus fractures are impacted, they are stable and rarely require manipulative reduction.
Torsional injuries result in two distinct patterns of fracture, depending on the maturity of the physis.
- In the very young child with a thick periosteum, the diaphyseal bone fails before the physis, resulting in a long spiral fracture.
- In the older child, similar torsional injury results in a physeal fracture.
Bending moments in the young child cause “greenstick fractures” in which the bone is incompletely fractured, resulting in a plastic deformity on the concave side of the fracture. The fracture may need to be completed to obtain an adequate reduction.
Bending moments can also result in microscopic fractures that create plastic deformation of the bone with no visible fracture lines on plain radiographs; permanent deformity can result.
In the older child, bending moments result in transverse or short oblique fractures. Occasionally, a small butterfly fragment may be seen; however, because pediatric bone fails more easily in compression, there may only be a buckle of the cortex.
CLINICAL EVALUATION
Pediatric trauma patients should undergo full trauma evaluation with attention to airway, breathing, circulation, disability, and exposure. This should ideally be performed under the direction of a general surgical trauma team or pediatric emergency specialist.
Children are not good historians; therefore, keen diagnostic skills may be required for even the simplest problems. Parents may not be present at the time of injury and cannot always provide an accurate history. It is important to evaluate the entire extremity, because young children cannot always localize the site of injury.
It is important to explain everything to children, listen to their suggestions whenever possible, and stop when they ask you to do so.
Neurovascular evaluation is mandatory, both before and after manipulation.
Periodic evaluation for compartment syndrome should be performed, particularly in a nonverbal patient who is irritable and who has a crush-type mechanism of injury. A high index of suspicion should be followed by compartment pressure monitoring.
Intracompartmental blood loss from long bone fractures of the lower extremities can be a serious problem for the young child.
Child abuse must be suspected in the following scenarios:
- Transverse femur fracture in a child <1 year old or a transverse humerus fracture in a child <3 years old.
- Metaphyseal corner fractures (caused by a traction/rotation mechanism).
- A history (mechanism of injury) that is inconsistent with the fracture pattern.
- An unwitnessed injury that results in fracture.
- Multiple fractures in various stages of healing.
- Skin stigmata suggestive of abuse: multiple bruises in various stages of resolution, cigarette burns, etc.
It is the obligation of the physician to ensure that the child is in a safe environment. If there is any question of abuse, the child should be admitted to the hospital and social services notified.
RADIOGRAPHIC EVALUATION
Radiographs should include appropriate orthogonal views of the involved bone as well as the joint proximal and distal to the suspected area of injury. If the location of the suspected injury is uncertain, the entire extremity may be placed on the radiographic plate.
A thorough understanding of normal ossification patterns is necessary to adequately evaluate plain radiographs.
Comparison views of the opposite extremity may aid in appreciating subtle deformities or in localizing a minimally displaced fracture. These should be obtained only when there is a question about the presence of a fracture seen on a radiograph of an injured extremity and not as a routine.
“Soft signs,” such as the posterior fat pad sign in the elbow, should be closely evaluated.
A skeletal survey may be helpful in searching for other fractures in cases of suspected child abuse or multiple traumas.
Computed tomography may be useful in evaluating complicated intra-articular fractures in the older child.
Magnetic resonance imaging can be valuable in the preoperative evaluation of a complicated fracture; it may also help evaluate a fracture not clearly identifiable on plain films due to lack of ossification.
Arthrograms are valuable in the intraoperative assessment of intra-articular fractures because radiolucent cartilaginous structures will not be apparent on fluoroscopic or plain radiographic evaluation.
Bone scans may be used in the evaluation of osteomyelitis or tumor.
Ultrasound can be useful for identifying epiphyseal separation in infants.
CLASSIFICATION
Pediatric physeal fractures have traditionally been described by the five-part Salter-Harris classification. The Ogden classification has extended the Salter-Harris classification to include periphyseal fractures, which do not radiographically appear to involve the physis but may interfere with the physeal blood supply and result in growth disturbance.

- Salter-Harris Types I to V
- Type I: Transphyseal fracture involving the hypertrophic and calcified zones. Prognosis is usually excellent because of the preservation of the reserve and proliferative zones, although complete or partial growth arrest may occur in displaced fractures. Radiographs may be unremarkable and the diagnosis is “clinical” based on physical examination.
- Type II: Transphyseal fracture that exits through the metaphysis. The metaphyseal fragment is known as the Thurston-Holland fragment. The periosteal hinge is intact on the side with the metaphyseal fragment. Prognosis is excellent, although complete or partial growth arrest may occur in displaced fractures.
- Type III: Transphyseal fracture that exits the epiphysis, causing intra-articular disruption as well as disrupting the reserve and proliferative zones. Anatomic reduction and fixation without violating the physis are essential. Prognosis is guarded, because partial growth arrest and resultant angular deformity are common problems.
- Type IV: Fracture that traverses the epiphysis and the physis, exiting the metaphysis and disrupting all four zones of the physis. Anatomic reduction and fixation without violating the physis are essential. Prognosis is guarded, because partial growth arrest and resultant angular deformity are common.
- Type V: Crush injury to the physis. Diagnosis is generally made retrospectively. Prognosis is poor, because growth arrest and partial physeal closure are common.
- Ogden Types VI to IX
- Type VI: Injury to the perichondral ring at the periphery of the physis. Usually, this is the result of an open injury. Close follow-up may allow early identification of a peripheral physeal bar that is amenable to excision. Prognosis is guarded, because peripheral physeal bridges are common.
- Type VII: Fracture involving the epiphysis only. This includes osteochondral fractures and epiphyseal avulsions. Prognosis is variable and depends on the location of the fracture and the amount of displacement.
- Type VIII: Metaphyseal fracture. Primary circulation to the remodeling region of the cartilage cell columns is disrupted. Hypervascularity may cause angular overgrowth.
- Type IX: Diaphyseal fracture. The mechanism for appositional growth (the periosteum) is interrupted. Prognosis is generally good if reduction is maintained. Cross-union between the tibia and fibula and between the radius and ulna may occur if there is intermingling of the respective periosteums.
TREATMENT
Fracture management in the child differs from that in an adult owing to the presence of a thick periosteum in the case of a diaphyseal fracture or open physis in metaphyseal fractures.
The tough periosteum can be an aid to reduction because the periosteum on the concave side of the deformity is usually intact and can be made to serve as a hinge, preventing overreduction. Longitudinal traction will not reliably unlock the fragments when the periosteum is intact. Controlled recreation and exaggeration of the fracture deformity are effective means of disengaging the fragments to obtain reduction.
A periosteal flap entrapped in the fracture site or buttonholing of a sharp fracture end through the periosteum can prevent an adequate reduction.
Remanipulation of physeal injuries should not be attempted after 5 to 7 days.
Unlike in the adult, considerable fracture deformity may be permitted because the remodeling potential of the young child is great.
In general, the closer the fracture is to the joint (physis), the better the deformity is tolerated (e.g., 45 to 60 degrees of angulation in a proximal humeral fracture in a young child is permissible, whereas the midshaft fracture of the radius or tibia should be brought to within 10 degrees of normal alignment).
Rotational deformity does not spontaneously correct or remodel to an acceptable extent even in the young child and should be avoided.
Severely comminuted or shortened fractures may require skin or skeletal traction. Traction pins should be placed proximal to the nearest distal physis (e.g., distal femur). Care should be taken not to place the traction pin through the physis.
Fracture reduction should be performed under conscious sedation, followed by immobilization in either a splint or bivalved cast. Univalving, particularly with a fiberglass cast, does not provide adequate cast flexibility to accommodate extremity swelling.
In children, casts or splints should encompass the joint proximal and distal to the site of injury, because postimmobilization stiffness is not a common problem for children. Only in rare fractures should short arm or short leg casts be applied initially as opposed to longer immobilization techniques (e.g., stable torus fractures of the distal radius).
In some cases, as soon as 2 days after cast application, children will run on short leg casts or climb monkey bars in short arm casts.
All fractures should be elevated at above the heart level, iced, and frequently monitored by responsible individuals, with attention to extremity warmth, color, capillary refill, and sensation. Patients in whom pronounced swelling is an issue or for whom the reliability of the guardian is in question should be admitted to the hospital for observation.
Fractures in which a reduction cannot be achieved or maintained should be splinted and the child prepared for general anesthesia, with which complete relaxation may be achieved.
Intra-articular fractures, Salter-Harris types III and IV, require anatomic reduction (<1 to 2 mm of displacement both vertically and horizontally) to restore articular congruity and to minimize physeal bar formation.
Indications for open reduction include:
- Most open fractures.
- Displaced intra-articular fractures (Salter-Harris types III and IV).
- Fractures with vascular injury.
- Fractures with an associated compartment syndrome.
- Unstable fractures that require abnormal positioning to maintain closed reduction.
COMPLICATIONS
Complications unique to pediatric fractures include the following:
- Complete growth arrest: This may occur with physeal injuries in Salter-Harris fractures. It may result in limb length inequalities necessitating the use of orthotics, prosthetics, or operative procedures includingepiphysiodesis or limb lengthening.
- Overgrowth may be seen in certain pediatric fractures such as femoral diaphysis.
- Progressive angular or rotational deformities: They may result from physeal injuries with partial growth arrest or malunion. May occur in certain metaphyseal fractures such as the proximal tibia. If these result in significant functional disabilities or cosmetic deformity, they may require operative intervention, such as osteotomy, for correction.
- Osteonecrosis: May result from disruption of tenuous vascular supply in skeletally immature patients in whom vascular development is not complete (e.g., osteonecrosis of the femoral head in cases of slipped capital femoral epiphysis).
1. What is the traditional physis division?
Answer: The physis is traditionally divided into four zones: reserve (resting/germinal), proliferative, hypertrophic, and provisional calcification (or enchondral ossification).
2. What is the incidence of pediatric fractures?
Answer: Approximately 50% of all children will fracture at least one bone during childhood.
3. What is the mechanism of injury for greenstick fractures?
Answer: Bending moments in the young child cause “greenstick fractures” in which the bone is incompletely fractured, resulting in a plastic deformity on the concave side of the fracture. The fracture may need to be completed to obtain an adequate reduction.

