Intramedullary Fixation of Clavicle Fractures
DEFINITION
■ The clavicle is one of the most commonly fractured bones.
■ The site on the clavicle most often fractured is the middle third.9
■ The midclavicular region is the thinnest and narrowest portion of the bone.
■ It is the only area not supported by ligament or muscle attachments.
■ It represents a transitional region of both cross-sectional anatomy and curvature.
■ It is the transition point between the lateral part, with a flatter cross section, and the more tubular medial.
■ Because of the clavicle’s S shape, an axial load creates a very high tensile force along the anterior midcortex. (Axial load makes a virtual right angle at midclavicle.)
ANATOMY
■ The clavicle is the only long bone to ossify by a combination of intramembranous and endochondral ossification.6
■ Its configuration is S-shaped, a double curve; the medial curve is apex anterior and the lateral curve is apex posterior (FIG 1A).
■ The larger medial curvature widens the space for the neu-
rovascular structures, providing bony protection.
■ The clavicle is made up of very dense trabecular bone, lack- ing a well-defined medullary canal.
■ The cross-sectional anatomy gradually changes from flat lat- erally, to tubular in the midportion, to expanded prismatic medially.
■ The clavicle is subcutaneous throughout, covered by the thin platysma muscle.
■ The supraclavicular nerves that provide sensation to the over- lying skin of the clavicle are found deep to the platysma muscle.
■ Very strong capsular and extracapsular ligaments attach the medial end to the sternum and first rib and the lateral end to the acromion and coracoid.
■ Proximal muscle attachments include the sternocleidomas- toid, pectoralis major, and subclavius. Distal muscle attach- ments include the deltoid and trapezius (FIG 1B).
■ The clavicle functions by providing a fixed-length strut
through which the muscles attached to the shoulder girdle can generate and transmit large forces to the upper extremity.
PATHOGENESIS
■ The mechanism of clavicle fractures in the vast majority is a direct injury to the shoulder.10 Stanley and associates studied
106 injured patients; 87% had fallen onto the shoulder, 7% were injured by a direct blow on the point of the shoulder, and only 6% reported falling onto an outstretched hand.
■ Stanley suggests that in the patients who described hitting the ground with an outstretched hand, the shoulder became the next contact point with the ground, causing the fracture. Stanley
Articular cartilage (AC joint)
stated that a compressive force equivalent to body weight would exceed the critical buckling load to cause the clavicle fracture.
NATURAL HISTORY
■ In the 1960s, both Neer7 and Rowe9 published large series of midclavicle fractures, showing very low nonunion rate (0.1% and 0.8%) with closed treatment and a higher nonunion rate (4.6% and 3.7%) with operative treatment.
■ More recent studies have shown that nonunion is more common then previously recognized and that a significant per- centage of patients with nonunion are symptomatic.
■ Malunion with shortening greater than 15 to 20 mm has also been shown to be associated with significant shoulder dysfunction.
■ McKee and colleagues5 identified 15 patients with mal-
union of the midclavicle after closed treatment. All patients had shortening of more than 15 mm, all were symptomatic and unsatisfied, and all underwent corrective osteotomy. Postoperatively all 15 patients improved in terms of function and satisfaction.
■ Hill and associates4 reviewed 52 completely displaced mid-
shaft clavicle fractures and found that shortening of more than
20 mm had a significant association with nonunion and unsat- isfactory results.
■ Eskola and coworkers3 reported on 89 malunions of the
midclavicle, showing that shortening of more than 15 mm was associated with shoulder discomfort and dysfunction.
PATIENT HISTORY AND PHYSICAL FINDINGS
■ The diagnosis is usually straightforward and is based on ob- taining the mechanism of injury from a good history.
■ On visual inspection the examiner will frequently see no- table swelling or ecchymosis at the fracture site and possibly deformity of the clavicle, with drooping of the shoulder downward and forward if the fracture is significantly dis- placed. The skin is inspected for tenting at the fracture site and characteristic bruising and abrasions that might suggest a direct blow or seatbelt shoulder strap injury (FIG 2A,B).
■ Palpation over the fracture site will reveal tenderness, and
gentle manipulation of the upper extremity or clavicle itself may reveal crepitus and motion at the fracture site.
■ The amount of shortening is identified by clinically measur- ing the distance of a straight line (in centimeters) from both acromioclavicular joints to the sternal notch and noting the difference (FIG 2C).
■ It is important to perform a complete musculoskeletal and
neurovascular examination of the upper extremity and auscul-
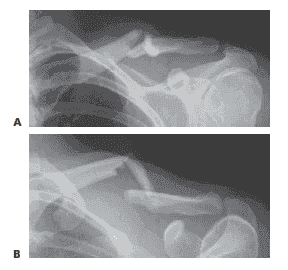 FIG 3 • Radiographs of the same displaced left clavicle fracture viewed from a standard AP projection (A) and a 45-degree cephalic tilt projection (B).
FIG 3 • Radiographs of the same displaced left clavicle fracture viewed from a standard AP projection (A) and a 45-degree cephalic tilt projection (B).tation of the chest to identify the rare associated injuries; these are more closely related to high-energy injuries.
■ Rib and scapula fracture
■ Brachial plexus injury (usually traction to upper cervical root)
■ Vascular injury (subclavian artery or vein injury associ- ated with scapulothoracic dissociation)
■ Pneumothorax and hemothorax
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Two orthogonal radiographic projections are necessary to determine the fracture pattern and displacement, ideally 45- degree cephalic tilt and 45-degree caudad tilt views.
■ Usually a standard anteroposterior (AP) view and a 45- degree cephalic tilt (FIG 3) view are adequate.
■ In practice, a 20- to 60-degree cephalic tilt view will min-
imize interference of thoracic structures.
■ The film should be large enough to include the acromioclav- icular and sternoclavicular joints, the scapula, and the upper lung fields to evaluate for associated injuries.
■ An AP view of bilateral clavicles on a wide cassette to in- clude the acromioclavicular joints and sternum is fairly helpful in determining the amount of shortening; however, this is a multiplanar deformity and a CT scan would have greater ac- curacy, although it is rarely required.
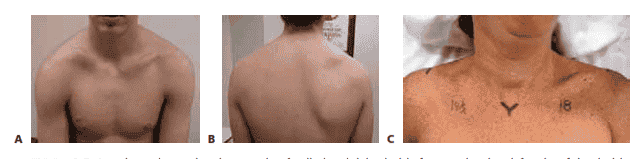 FIG 2 • A,B. Anterior and posterior photographs of a displaced right clavicle fracture showing deformity of the clavicle and drooping of the shoulder girdle downward and forward. C. Clinical picture of a displaced right clavicle fracture, showing 3.5 cm of shortening, measured from the sternal notch to the acromioclavicular joint.
FIG 2 • A,B. Anterior and posterior photographs of a displaced right clavicle fracture showing deformity of the clavicle and drooping of the shoulder girdle downward and forward. C. Clinical picture of a displaced right clavicle fracture, showing 3.5 cm of shortening, measured from the sternal notch to the acromioclavicular joint.
DIFFERENTIAL DIAGNOSIS
■ Sprain of acromioclavicular joint
■ Sprain of sternoclavicular joint
■ Rib fracture
■ Muscle injury
■ Contusion
■ Hematoma
■ Kehr sign: referred pain to the left shoulder from irritation of the diaphragm, signaled by the phrenic nerve. Irritation may be caused by diaphragmatic or peridiaphragmatic lesions, renal calculi, splenic injury, or ectopic pregnancy.
NONOPERATIVE MANAGEMENT
■ If the clavicle fracture alignment is acceptable, generally a simple configuration with less than 15 mm of shortening, then any of a number of methods of supporting the upper extrem- ity are adequate, including a figure 8 bandage, sling, sling and swathe, Sayre bandage, Velpeau dressing, and benign neglect, just to name a few.
■ Nordqvist and colleagues8 reported on 35 clavicle fracture
malunions with shortening of less than 15 mm. They were all treated nonoperatively in a sling. All 35 had normal mobility, strength, and function compared to the normal shoulder.
■ A prospective, randomized study2 comparing sling versus
figure 8 bandage showed that a greater percentage of patients were dissatisfied with the figure 8 bandage, and there was no difference in overall healing and alignment. The study concluded that the figure 8 bandage does little to obtain reduction.
SURGICAL MANAGEMENT
■ Indications for operative treatment of acute midshaft clavi- cle fractures are as follows:
■ Open fractures
■ Fractures with neurovascular injury
■ Fractures with severe associated chest injury or multiple trauma: patients who require their upper extremity for transfer and ambulation
■ “Floating shoulder”
■ Impending skin necrosis
■ Severe displacement: possibly 15 to 20 mm of shortening
■ In a multicenter, randomized, prospective clinical trial of displaced midshaft clavicle fractures, Altamimi and McKee1 showed that operative fixation compared to nonoperative treatment improved functional outcome and had a lower rate of both malunion and nonunion.
■ Potential advantages of intramedullary fixation of the clavi- cle are as follows:
■ Less soft tissue stripping and therefore potentially better healing
■ Smaller incision
■ Better cosmesis
■ Easier hardware removal
■ Less weakness of bone after hardware removal
■ Potential disadvantages of intramedullary fixation of the clavicle are as follows:
■ Less ability to resist torsional forces
■ Skin breakdown from prominence distally
■ Pin breakage
■ Pin migration
■ Newer designs and techniques prevent pin migration by placing a locking nut on the lateral end and technically avoid- ing penetration of the medial fragment cortex.
Preoperative Planning
■ After the decision has been made to fix a clavicle fracture, one must evaluate whether the fracture pattern is amenable to intramedullary pin fixation.
■ A simple fracture pattern in the middle third of the bone is ideal.
■ The fracture should not extend past the middle third of the bone.
■ Comminution and butterfly fragments (usually anterior) are common and do not preclude intramedullary fixation as long as the medial and distal main fragments have cortical contact.
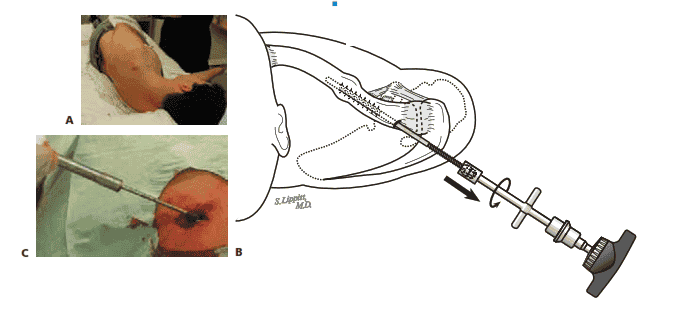
Positioning
■ There are two good options for patient positioning that fa- cilitate use of an image intensifier or C-arm device, which will aid you during pin placement.
■ The patient can be placed supine on a Jackson radiolucent surgical table so the C-arm can be brought in perpendicular from the opposite side of the table, which is out of the way of the surgeon (FIG 4A,B).
FIG 4 • A,B. The patient is placed supine on a Jackson radiolucent surgical table. A 1-L bag is placed under the affected shoul- der, medial to the scapula, and the arm is prepared free and placed in an arm holder to aid in fracture reduction. The C-arm can be brought in perpendicular from the opposite side of the table, which is out of the way of the surgeon and facilitates getting orthogonal radiographic views of the fracture: 45-degree caudad tilt view (A) and 45-degree cephalic tilt view
(B). C,D. Alternatively, the patient is placed in the beach chair position on the OR table, using a radiolucent shoulder-position-
ing device. C. The arm is prepared free and placed in an arm holder to facilitate fracture reduction. The C-arm is brought in from the head of the bed with the gantry rotated upside down and slightly away from the operative shoulder and oriented with a cephalic tilt. D. The same beach chair positioning shown sterilely draped.
■ A 1-L bag is placed under the affected shoulder, medial to the scapula, to aid in fracture reduction.
■ The arm is also prepared free and placed in an arm holder to facilitate fracture reduction.
■ This is our preferred method due to the ease and speed of the set-up and the ease of getting orthogonal radiographic views of the fracture (45-degree cephalic and caudad tilt views).
■ The other option is placing the patient in the beach chair po- sition on the OR table, using a radiolucent shoulder- positioning device (FIG 4C,D).
■ The C-arm is brought in from the head of the bed with the
gantry rotated upside down and slightly away from the operative shoulder and oriented with a cephalic tilt.
■ The arm is also prepared free and placed in an arm holder to facilitate fracture reduction.
INCISION AND DISSECTION
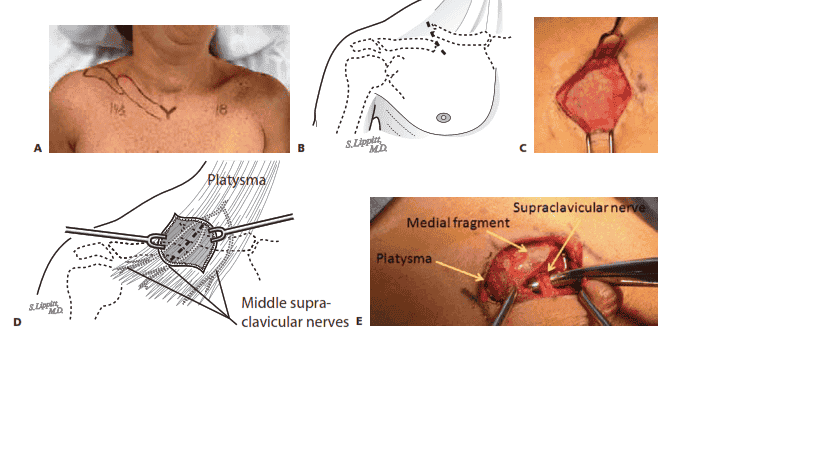
■ Mark out the clavicle, fracture site, and surrounding anatomy (TECH FIG 1A).
■ Use the C-arm to identify the appropriate position for
the incision, which should be over the distal end of the medial fragment, in the Langer lines of the normal skin crease around the neck (TECH FIG 1B).
■ Make an incision of about 2 to 3 cm over the fracture site.
■ Divide the subcutaneous fat down to the platysma mus- cle using electrocautery (TECH FIG 1C).
■ Although there is usually very little subcutaneous fat,
gently make full-thickness flaps to include skin and sub- cutaneous tissue around the entire incision to facilitate exposure.
■ Bluntly split the platysma muscle in line of its fibers to
identify, protect, and retract the underlying supraclavic-
ular nerves; its middle branches are frequently found near the midclavicle (TECH FIG 1D,E).
■ The fracture site is then usually easily identifiable in
acute injuries because the periosteum is disrupted and usually requires no further division.
■ Remove any debris, hematoma, or interposed muscle
from the fracture site.
■ If there are butterfly fragments, be careful to keep any soft tissue attachments.
TECH FIG 1 • A. Displaced right clavicle fracture, showing the clavicle and fracture site marked out. B. A skin incision of about
2 to 3 cm is made over the distal end of the medial clavicular fragment, in the Langer lines of normal skin creases around the neck. C. Incision over a clavicle fracture site, showing full-thickness flaps to include skin and subcutaneous tissue around the en- tire incision. This exposes the fascia that covers the platysma muscle. D. Skin incision over a displaced clavicle fracture, with un- derlying platysma muscle and the middle supraclavicular nerves. E. Intraoperative photo showing the platysma muscle bluntly split in the line of its fibers to identify an underlying supraclavicular nerve, which is under the clamp. The fracture site is usually easily identifiable in acute injuries because the periosteum is disrupted and usually requires no further division; as shown here, the medial clavicular fragment is easily seen. (B,D: Courtesy of Steven B. Lippitt, MD.)
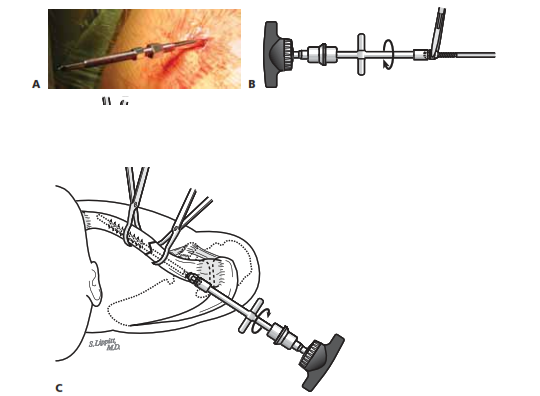
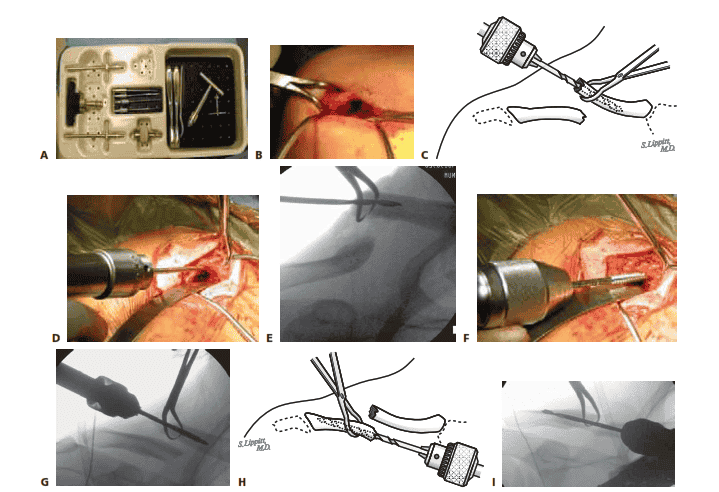
CLAVICLE PREPARATION
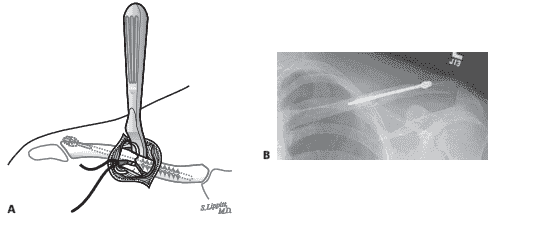
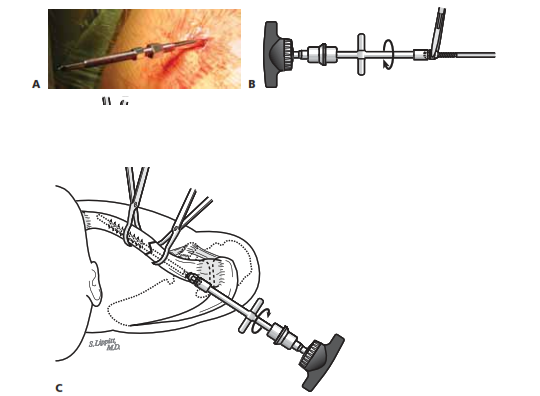
■ The following technique uses a modified Hagie pin called the Rockwood Clavicle Pin (DePuy Orthopaedics, Warsaw, IN) (TECH FIG 2A).
■ Use a bone-reducing clamp or towel clip to grab and el-
evate the medial clavicular fragment through the inci- sion (TECH FIG 2B).
■ Size the diameter of the canal with the appropriate-size
drill bit; the C-arm can be useful to judge canal fill and orientation of the drill.
■ The fit should be snug to maximize fixation, but not
too tight, to prevent splitting the bone.
■ Attach the chosen drill to the T-handle and ream out the intramedullary canal without penetrating the anterior cortex (TECH FIG 2C–E).
■ Next, attach the appropriate-sized tap (that corre-
sponds to the drill size) to the T-handle and tap the
intramedullary canal to the anterior cortex (TECH FIG 2F,G).
■ Elevate the lateral clavicular fragment through the inci- sion; this can be facilitated by externally rotating the arm.
■ Use the same drill bit attached to the T-handle to ream
out the lateral fragment, but this time, under C-arm guidance, penetrate the posterolateral cortex of the clavicle (TECH FIG 2H,I).
■ The drill should exit posterior and medial to the
acromioclavicular joint capsule (TECH FIG 2J).
■ To prevent the pin nuts from being too prominent, make sure the drill does not exit in the upper half of the posterolateral clavicle.
■ Attach the appropriate-sized tap to the T-handle and tap
the intramedullary canal of the lateral fragment (TECH FIG 2K).
TECH FIG 2 • A. The Rockwood Clavicle Pin instrument set by DePuy Orthopaedics, Warsaw, IN, which is a modified Hagie pin. B. A bone-reducing clamp is used to elevate the medial clavicular fragment through the incision. C–E. The chosen drill is attached to a T-handle and the intramedullary canal of the medial clavicular fragment is reamed without penetrating the anterior cortex. F,G. An appropriate-sized tap is attached to a T-handle and the intramedullary canal of the medial clavicular fragment is tapped to the anterior cortex. H,I. The chosen drill is attached to a T-handle and the intramedullary canal of the lateral clavicular fragment is reamed out, penetrating the posterolateral cortex under direct C-arm guidance. (continued)
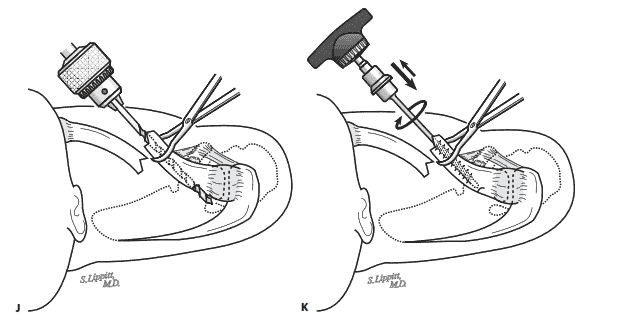 K
K
TECH FIG 2 • (continued) J. When drilling out the posterolateral cortex of the lateral clavicular fragment, the drill should exit posterior and medial to the acromioclavicular joint capsule. To prevent the pin nuts from being too prominent, the drill should not exit in the upper half of the posterolateral clavicle. K. The appropriate- sized tap is attached to the T-handle and the intramedullary canal of the lateral fragment is tapped. (C,H,J,K: Courtesy of Steven B. Lippitt, MD.)
PIN INSERTION AND FRACTURE REDUCTION
■ Remove the nuts from the pin assembly and attach the T-handle using a Jacobs chuck to the medial end of the clavicle pin.
■ This is the end with the large threads.
■ Never tighten the chuck over the machined threads at either end.
■ Continue firmly holding the lateral fragment while pass-
ing the trocar end (lateral end) of the clavicle pin into the intramedullary canal, out the previously drilled hole in the posterolateral cortex (TECH FIG 3A).
■ Once you are just through the cortex, make a small inci-
sion over the palpable tip.
■ Bluntly dissect the subcutaneous tissue with a hemostat until the tip of the pin can be felt, and then place the
hemostat or a small elevator under the tip of the pin to facilitate the pin’s passage through the incision (TECH FIG 3B).
■ Drill the pin out laterally until the large medial
threads engage the lateral fragment.
■ Now switch the T-handle to the lateral end of the pin and retract the pin into the lateral fragment (TECH FIG 3C,D).
■ Reduce the fracture by lifting the arm, and pass the pin
into the medial fragment.
■ Use the C-arm to ensure that the pin advances correctly down the line of the medial fragment and that all the medial threads cross the fracture site.
 TECH FIG 3 • A. The surgeon continues firmly holding the lateral fragment while passing the trocar end (lateral end) of the clavicle pin into the intramedullary canal, out the previously drilled hole in the pos- terolateral cortex. Once just through the cortex, the surgeon makes a small incision
TECH FIG 3 • A. The surgeon continues firmly holding the lateral fragment while passing the trocar end (lateral end) of the clavicle pin into the intramedullary canal, out the previously drilled hole in the pos- terolateral cortex. Once just through the cortex, the surgeon makes a small incisionA over the palpable tip. (continued)
B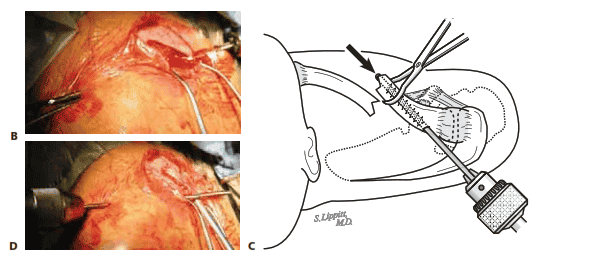
TECH FIG 3 • (continued) B. The subcutaneous tissue is bluntly dissected with a hemostat until the tip of the pin can be felt, and then the hemostat or a small elevator is placed under the tip of the pin to facilitate the pin’s passage through the incision. C,D. The T-handle is switched to the lateral end of the pin and the pin is retracted into the lateral fragment. (A,C: Courtesy of Steven B. Lippitt, MD.)
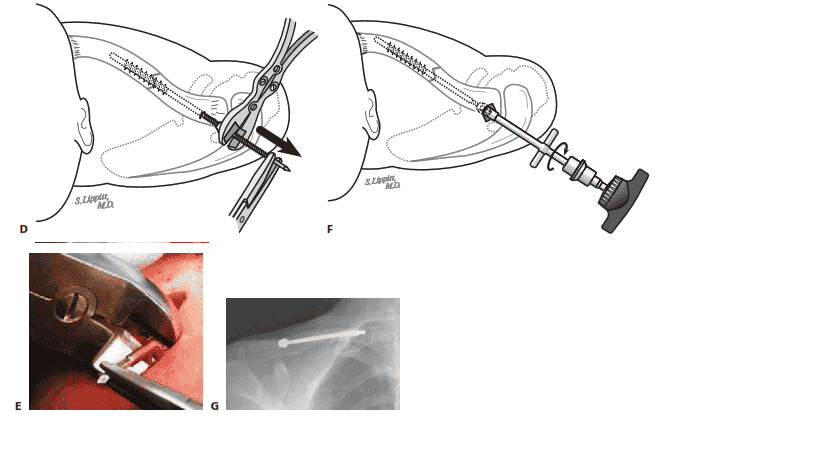
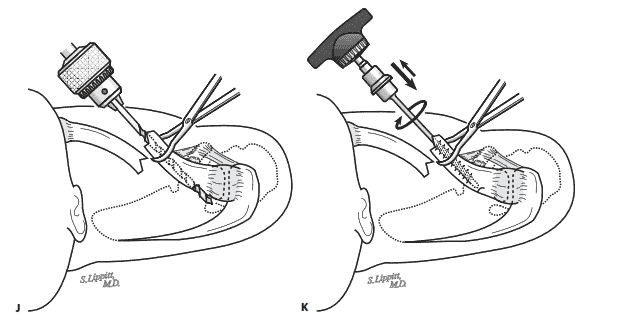
FINAL POSITIONING OF PIN AND FRACTURE COMPRESSION
■ Cold-weld the two nuts onto the lateral end of the pin.
■ First place the medial nut onto the pin, followed by the smaller lateral nut.
■ Grasp the medial nut with a needle-nose pliers and
then tighten the lateral nut against the medial nut using the lateral nut wrench (TECH FIG 4A,B).
■ Using the lateral nut wrench and C-arm guidance, now
advance the pin assembly into the medial fragment until it contacts the anterior cortex (TECH FIG 4C).
■ Break the cold weld by grasping the medial nut with
needle-nose pliers and then loosen the lateral nut by turning it counterclockwise using the lateral nut wrench.
■ Advance the medial nut against the posterolateral cor- tex of the clavicle to get desired compression across the fracture site.
■ Cold-weld the lateral nut back onto the medial nut
again.
■ Use the medial nut wrench to back the pin assembly out of the soft tissues far enough to expose the nuts, usually about 1 cm. This will enable the pin to be cut flush to the lateral nut (TECH FIG 4D,E).
■ Finally, use the lateral nut wrench to advance the pin
assembly back into the medial fragment with the same desired fracture site compression (TECH FIG 4F,G).
A B
 TECH FIG 4 • A. The lateral end of the pin with the larger medial nut is placed first, closest to the skin, followed by the smaller lat- eral nut, in preparation for cold welding. B. To cold weld the joint, the medial nut is grasped with a needle-nose pliers, and then the lateral nut is tightened against the medial nut using the lateral nut wrench. C. Using the lateral nut wrench and C-arm guidance, the surgeon advances the pin assembly into the medial fragment until it contacts the an-
TECH FIG 4 • A. The lateral end of the pin with the larger medial nut is placed first, closest to the skin, followed by the smaller lat- eral nut, in preparation for cold welding. B. To cold weld the joint, the medial nut is grasped with a needle-nose pliers, and then the lateral nut is tightened against the medial nut using the lateral nut wrench. C. Using the lateral nut wrench and C-arm guidance, the surgeon advances the pin assembly into the medial fragment until it contacts the an-C terior cortex. (continued)
TECH FIG 4 • (continued) D,E. The medial nut wrench is used to back the pin assembly out of the soft tissues far enough to expose the nuts, usually about 1 cm, to enable the pin to be cut flush to the lateral nut. F. The lateral nut wrench is used to advance the pin assem- bly back into the medial fragment with the same desired fracture site compression. G. Radiograph showing final positioning of the pin assembly with fracture site compression.
E G (B–D,F: Courtesy of Steven B. Lippitt, MD.)
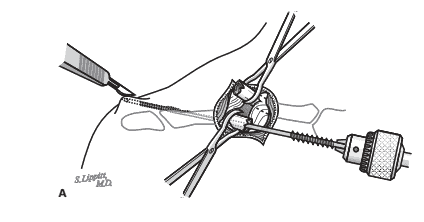
BUTTERFLY FRAGMENT MANAGEMENT AND WOUND CLOSURE
■ If an anterior butterfly fragment exists, cerclage is done using no. 0 or no. 1 absorbable suture.
■ Pass an elevator under the clavicle to deflect the su-
tures (TECH FIG 5A).
■ Then pass the suture in a figure 8 manner through the periosteum of the butterfly fragment and around the fragment and the clavicle (TECH FIG 5B).
■ Close the periosteum overlying the fracture site with no. 0
absorbable suture in an interrupted figure 8 manner.
■ Reapproximate the fascia of the platysma muscle using
2-0 absorbable suture in an interrupted figure 8 manner.
■ Close the subcutaneous tissue and skin of both incisions.
TECH FIG 5 • A. Cerclage of an anterior butterfly fragment is accomplished by first passing an elevator under the clavicle to deflect the sutures and then passing the suture, in a fig- ure 8 manner, through the periosteum of the butterfly fragment and around the fragment and the clavicle. B. Radiograph showing an adequate reduction of a butterfly fragment. (A: Courtesy of Steven B. Lippitt, MD.)
PIN REMOVAL
■ The pin is removed at 10 to 12 weeks if the fracture has healed.
■ The patient is positioned on his or her side and a local
anesthetic is delivered (TECH FIG 6A).
■ An incision is made over the same previous lateral inci- sion and the subcutaneous tissue is dissected using the hemostat until the medial nut is identified.
■ The medial nut wrench is used to extract the pin assem-
bly (TECH FIG 6B,C).
■ If the nut is stripped, the T-handle and chuck can be used to extract the pin assembly.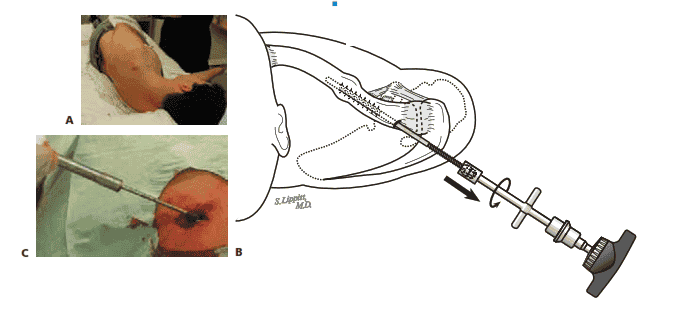
TECH FIG 6 • A. The patient is positioned on his or her side and the lateral incision is infiltrated with local anesthesia. B,C. The surgeon makes an incision over the same previous lateral inci- sion, dissecting through the subcutaneous tissue using the hemostat until the medial nut is iden- tified and freed up. The medial nut wrench is then used to extract the pin assembly. (B: Courtesy of Steven B. Lippitt, MD.)
PEARLS AND PITFALLS
Avoid splitting the clavicular fragments ■ If tapping the medial or lateral clavicular fragments is too tight, the surgeon and aid in pin insertion should redrill with the next larger drill size.
Achieve a more anatomic fracture reduction ■ When advancing the pin into the medial clavicular fragment, the surgeon should avoid starting too superior and anterior, which can lead to malreduc- tion. Instead, the pin should be inserted more inferior and posterior to achieve a more anatomic reduction.
POSTOPERATIVE CARE
■ A sling is worn for 4 weeks. During this time the sling is removed at least five times a day for active range of motion of the elbow and active assisted range of motion of the shoulder to 90 degrees of forward flexion.
■ The sling is discontinued and full active range of motion of the shoulder is started at 4 weeks.
■ Progressive resistance exercises are started at 6 weeks if the patient achieved full range of motion and there is clinical and radiographic evidence of healing.
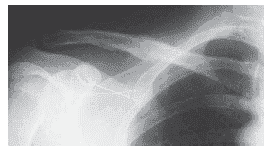
■ Once the clavicle fracture has healed, the pin is removed at 10 to 12 weeks, as described in the Techniques section (FIG 5).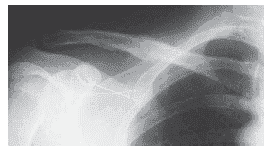
FIG 5 • Radiograph showing a healed clavicle fracture after pin assembly removal.
OUTCOMES
■ One of the authors (C.B.) has performed intramedullary fixa- tion of some 300 acute fractures; there have been 60 malunions and 30 nonunions of the clavicle, with a nonunion rate of 1.2%.
■ Most of the nonunions occurred in older, sick patients with polytrauma.
COMPLICATIONS
■ Pin migration is rare with this technique because of the locking nut on the lateral end of the pin, the blunt tip on the medial end of the pin, and technically avoiding penetration of the medial fragment cortex.
■ The risk of skin breakdown from pin prominence laterally can be minimized by making sure the drill exits the posterolat- eral clavicle in the lower half.
■ Neurovascular complications are rare.
■ There is no drilling toward the neurovascular structures with this technique.
■ When exposing the fracture site, the surgeon should stay on bone at all times.
■ Nonunion rates are low as long as general fracture princi- ples are maintained, soft tissue stripping of the fracture site is minimized, the technique is followed to get adequate fracture site compression and alignment, and the patient is compliant with the postoperative protocol.
■ Malunion can rarely occur, especially in fractures with large butterfly fragments. Good imaging with the C-arm allows the surgeon to start inserting the pin more inferior and posterior
down the line of the medial clavicular fragment to achieve a more anatomic reduction.
■ Infection is rare, especially with this technique, which has a relatively short surgical time and small exposure. Preoperative antibiotics, meticulous handling of the soft tissues, and ade- quate irrigation should be part of any surgical technique.
REFERENCES
1. Altamimi S, McKee M. Nonoperative treatment compared with plate fixation of displaced midshaft clavicle fractures. J Bone Joint Surg Am
2008;90A:1–8.
2. Andersen K, Jensen PO, Lauritzen J. Treatment of clavicular frac- tures: figure-of-eight versus a simple sling. Acta Orthop Scand 1987;
58:71–74.
3. Eskola A, Vainionpaa S, Myllynen P, et al. Outcome of clavicular frac- tures in 89 patients. Arch Orthop Trauma Surg 1986;105:337–338.
4. Hill J, McGuire M, Crosby L. Closed treatment of displaced middle- third fractures of the clavicle gives poor results. J Bone Joint Surg Br
1997;79B:537–539.
5. McKee M, Wild L, Schemitsch E. Midshaft malunions of the clavicle.
J Bone Joint Surg Am 2003;85A:790–797.
6. Moseley HF. The clavicle: its anatomy and function. Clin Orthop
Relat Res 1968;58:17–27.
7. Neer C. Nonunion of the clavicle. JAMA 1960;172:96–101.
8. Nordqvist A, Redlund-Johnell I, Von Scheele A, et al. Shortening of clavicle after fracture, incidence and clinical significance, a 5-year follow-up of 85 patients. Acta Orthop Scand 1997;68:349–351.
9. Rowe C. An atlas of anatomy and treatment of midclavicular frac- tures. Clin Orthop Relat Res 1968;58:29–42.
10. Stanley D, Trowbridge EA, Norris SH. The mechanism of clavicle fracture: a clinical and biomechanical analysis. J Bone Joint Surg Br
1988;70B:461–464.
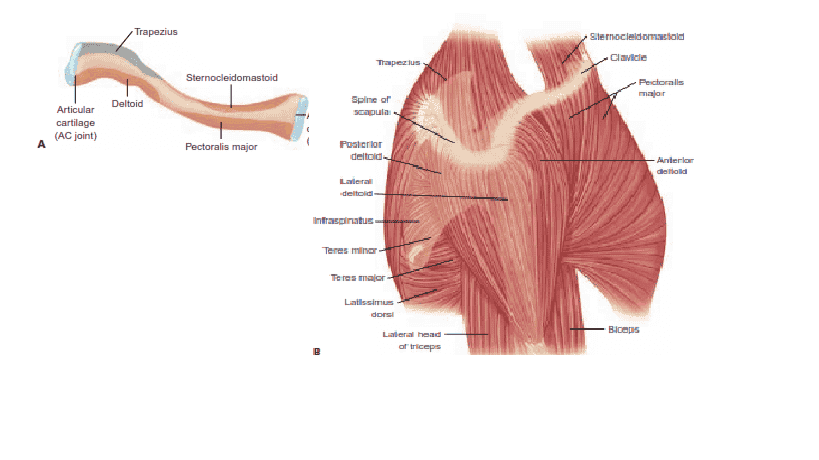
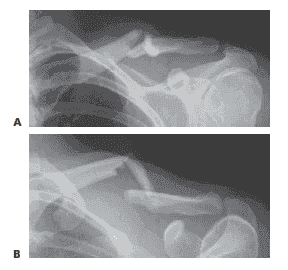 FIG 3 • Radiographs of the same displaced left clavicle fracture viewed from a standard AP projection (A) and a 45-degree cephalic tilt projection (B).
FIG 3 • Radiographs of the same displaced left clavicle fracture viewed from a standard AP projection (A) and a 45-degree cephalic tilt projection (B).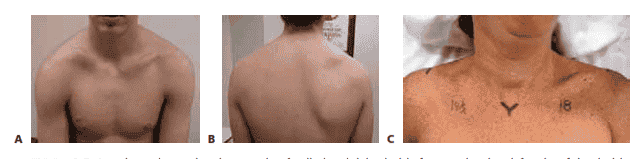 FIG 2 • A,B. Anterior and posterior photographs of a displaced right clavicle fracture showing deformity of the clavicle and drooping of the shoulder girdle downward and forward. C. Clinical picture of a displaced right clavicle fracture, showing 3.5 cm of shortening, measured from the sternal notch to the acromioclavicular joint.
FIG 2 • A,B. Anterior and posterior photographs of a displaced right clavicle fracture showing deformity of the clavicle and drooping of the shoulder girdle downward and forward. C. Clinical picture of a displaced right clavicle fracture, showing 3.5 cm of shortening, measured from the sternal notch to the acromioclavicular joint.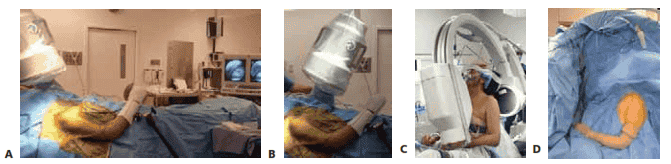
 K
K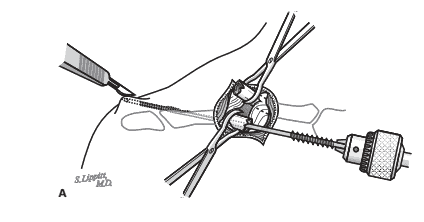 TECH FIG 3 • A. The surgeon continues firmly holding the lateral fragment while passing the trocar end (lateral end) of the clavicle pin into the intramedullary canal, out the previously drilled hole in the pos- terolateral cortex. Once just through the cortex, the surgeon makes a small incision
TECH FIG 3 • A. The surgeon continues firmly holding the lateral fragment while passing the trocar end (lateral end) of the clavicle pin into the intramedullary canal, out the previously drilled hole in the pos- terolateral cortex. Once just through the cortex, the surgeon makes a small incision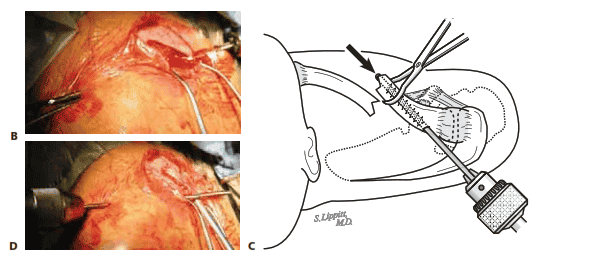
 TECH FIG 4 • A. The lateral end of the pin with the larger medial nut is placed first, closest to the skin, followed by the smaller lat- eral nut, in preparation for cold welding. B. To cold weld the joint, the medial nut is grasped with a needle-nose pliers, and then the lateral nut is tightened against the medial nut using the lateral nut wrench. C. Using the lateral nut wrench and C-arm guidance, the surgeon advances the pin assembly into the medial fragment until it contacts the an-
TECH FIG 4 • A. The lateral end of the pin with the larger medial nut is placed first, closest to the skin, followed by the smaller lat- eral nut, in preparation for cold welding. B. To cold weld the joint, the medial nut is grasped with a needle-nose pliers, and then the lateral nut is tightened against the medial nut using the lateral nut wrench. C. Using the lateral nut wrench and C-arm guidance, the surgeon advances the pin assembly into the medial fragment until it contacts the an-