افضل دكتور عظام For Doctors Proximal Humeral Fractures, Extra Articular 2-Part, Surgical Neck, Impaction Treatment Reverse Arthroplasty SURGICAL TECHNIQUE
1. Principles
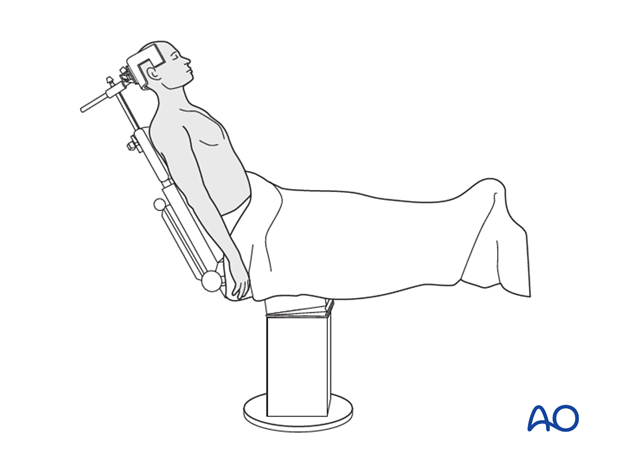
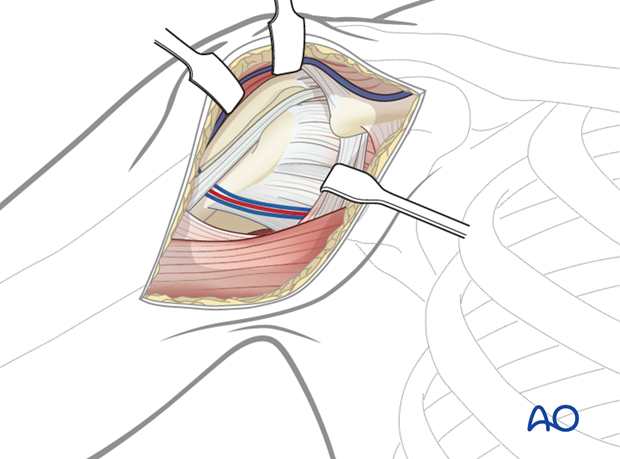
2. Patient preparation and approaches
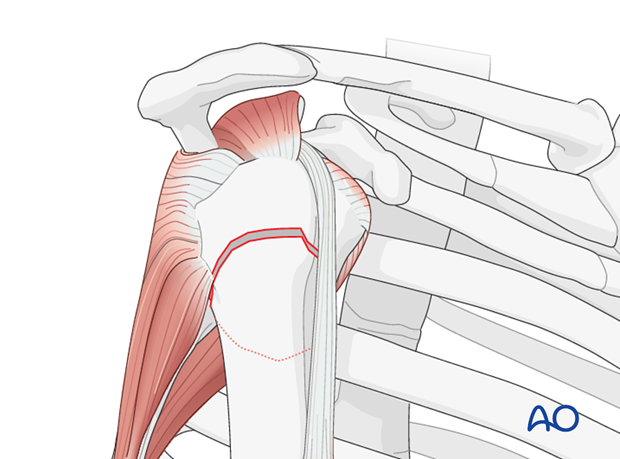
3. Evaluation of the fracture
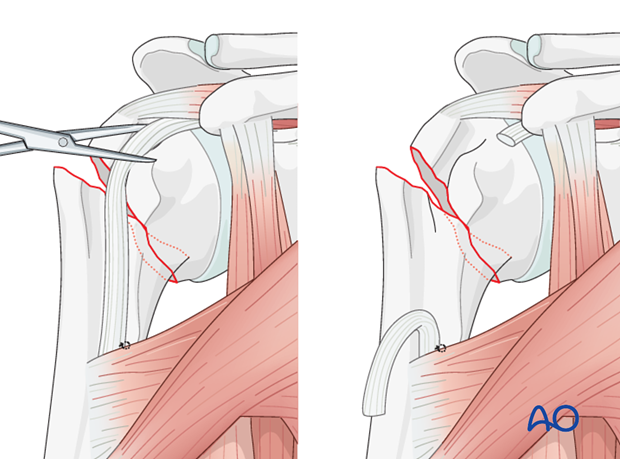
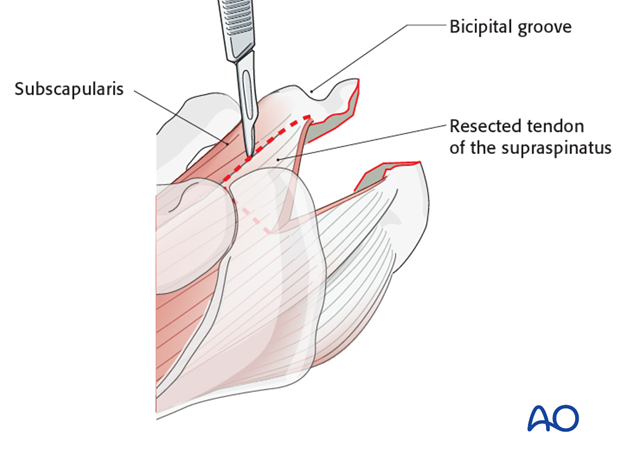
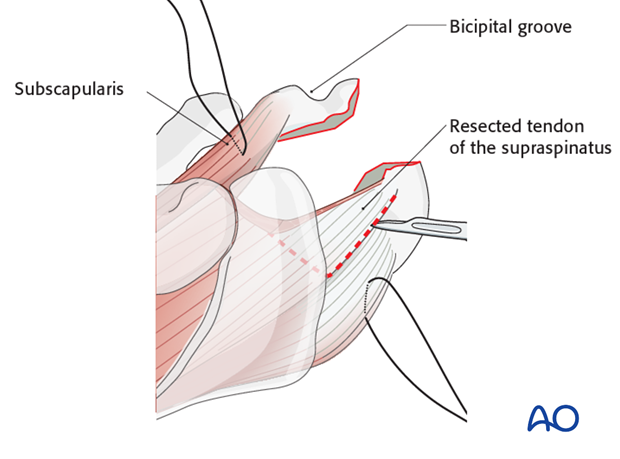
4. Tenotomy of the long head of the biceps
5. Surgical technique for two- or three-part fracture
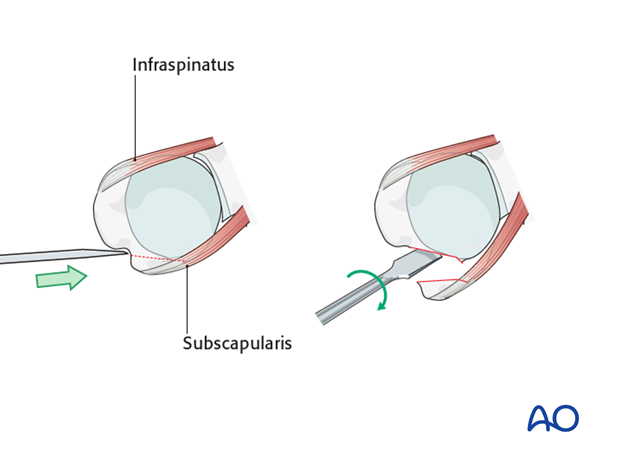
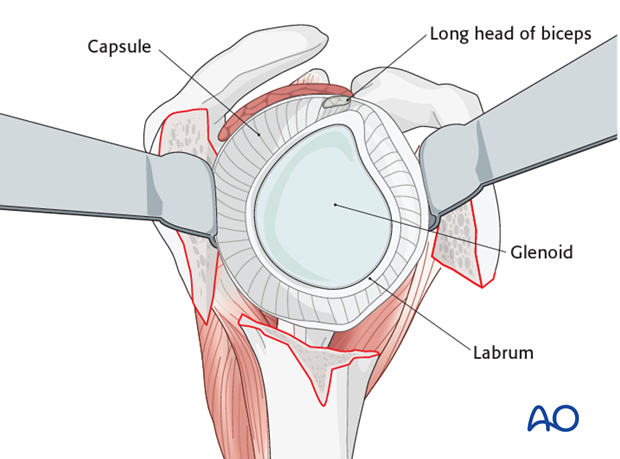
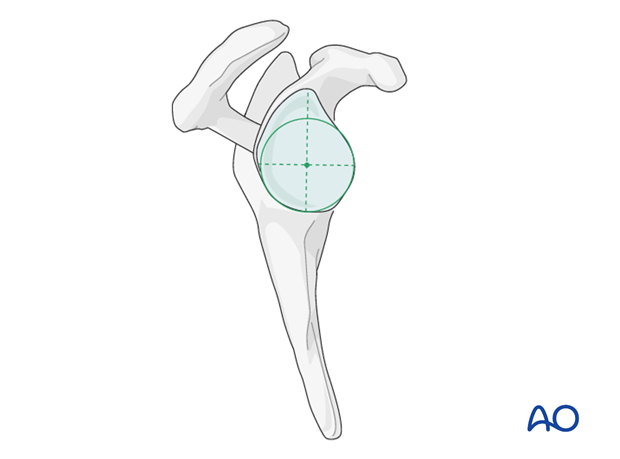
6. Preparation of the joint for placement of prosthesis


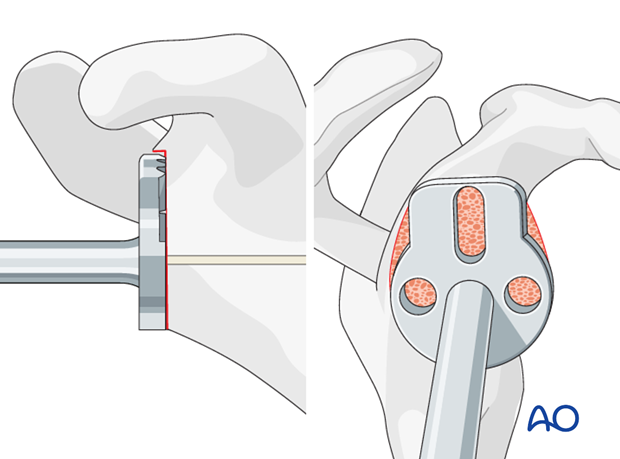
7. Glenoid surgical steps
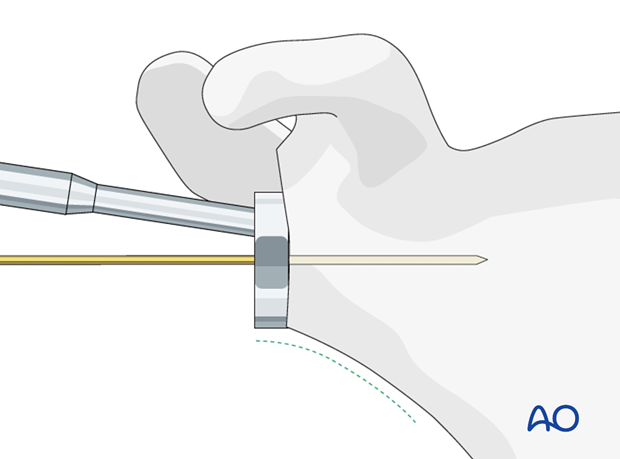
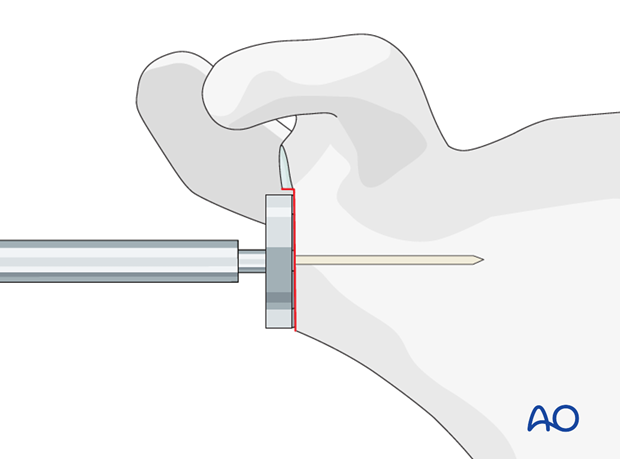
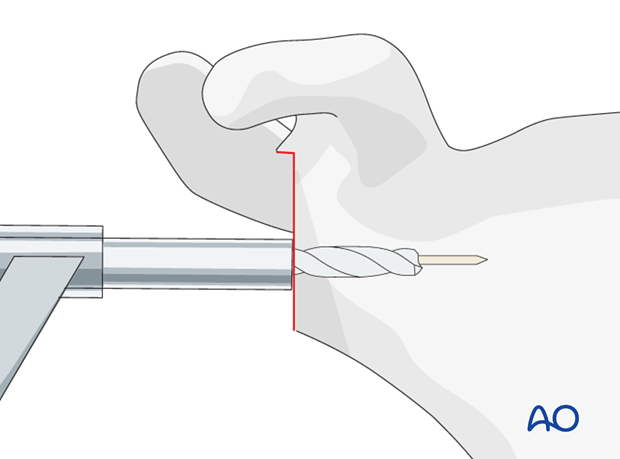
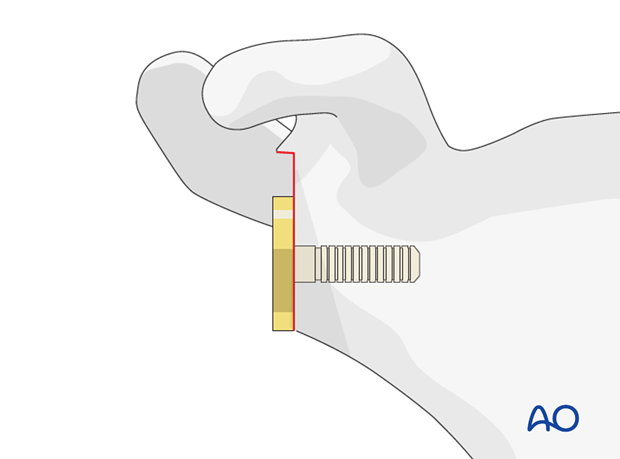
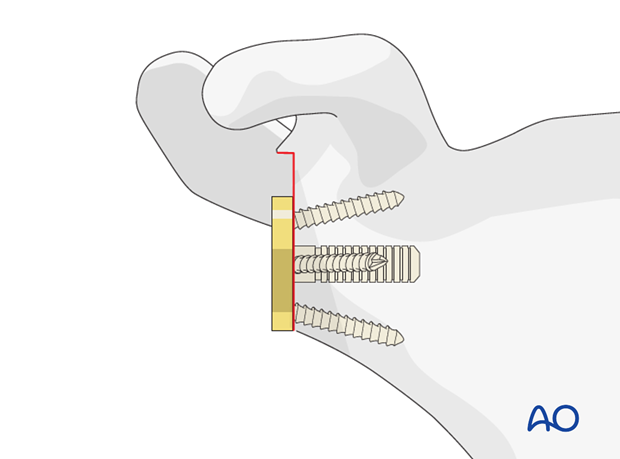
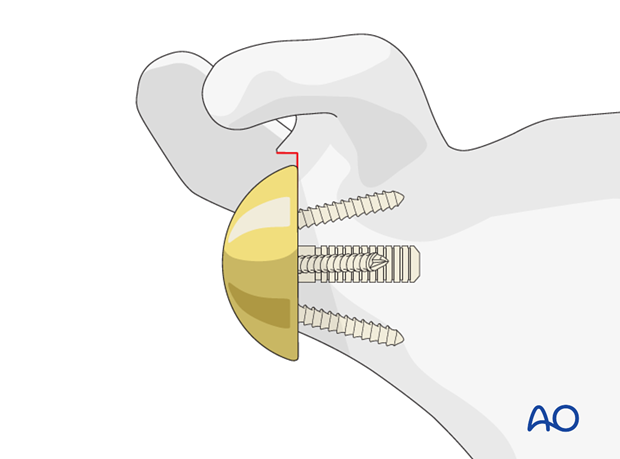
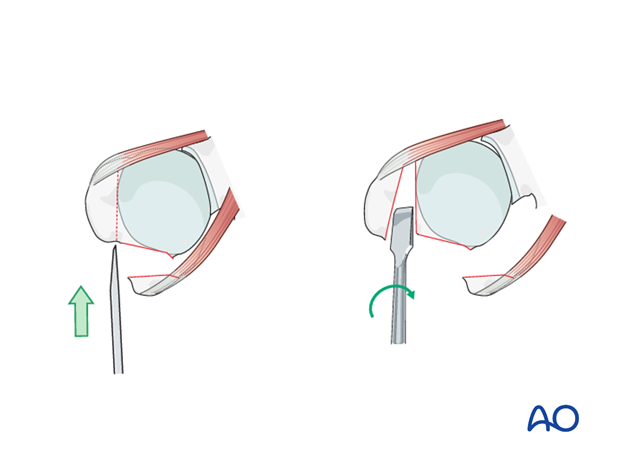
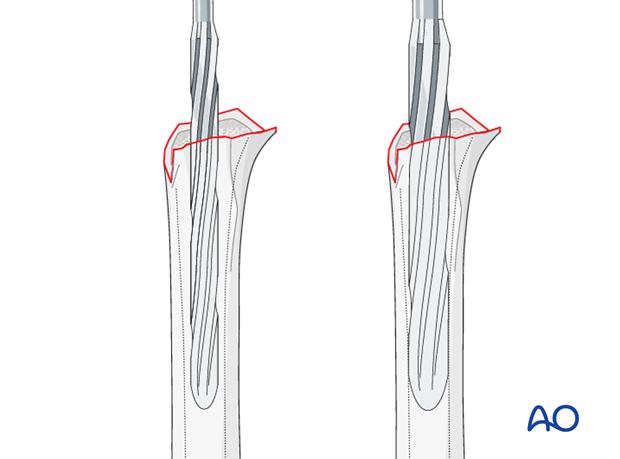
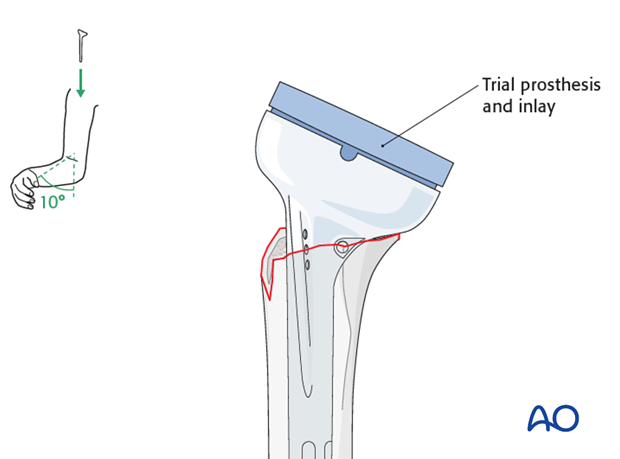
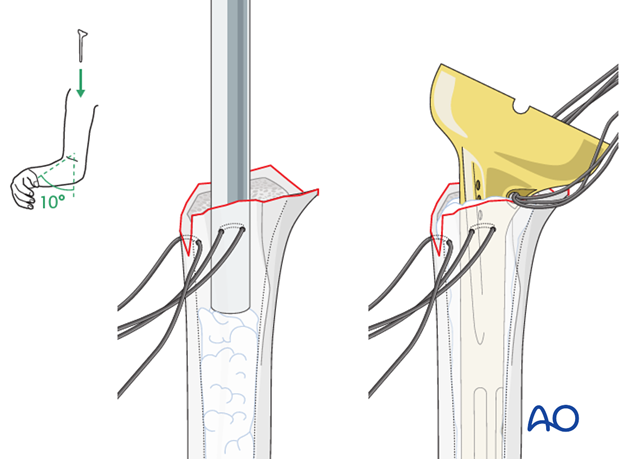
8. Humerus surgical steps
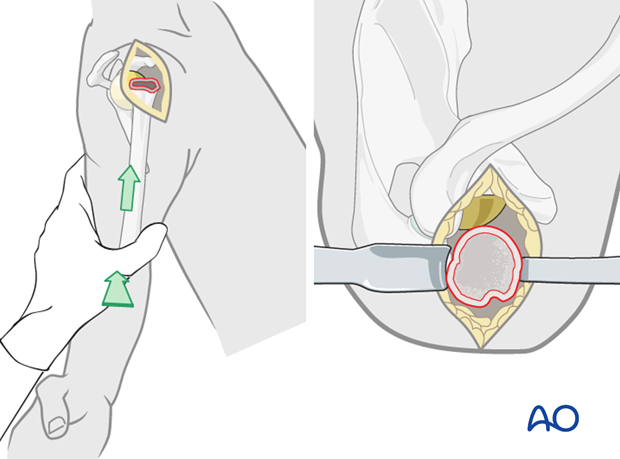
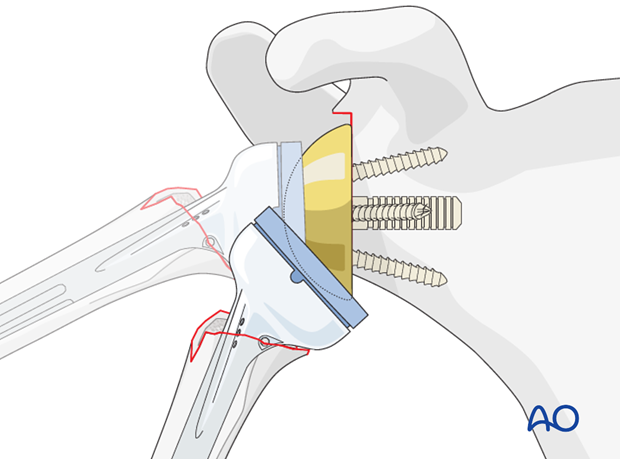
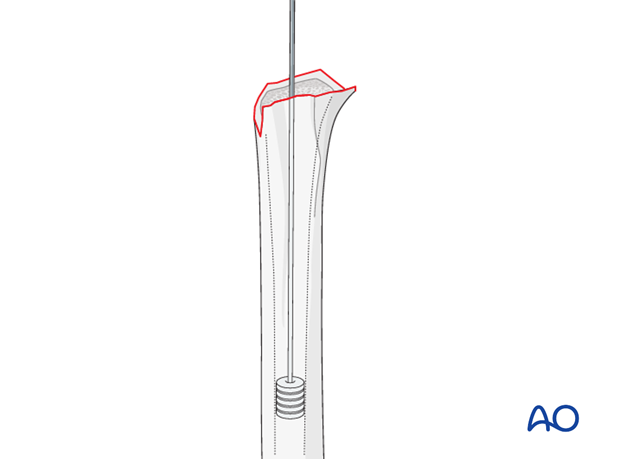


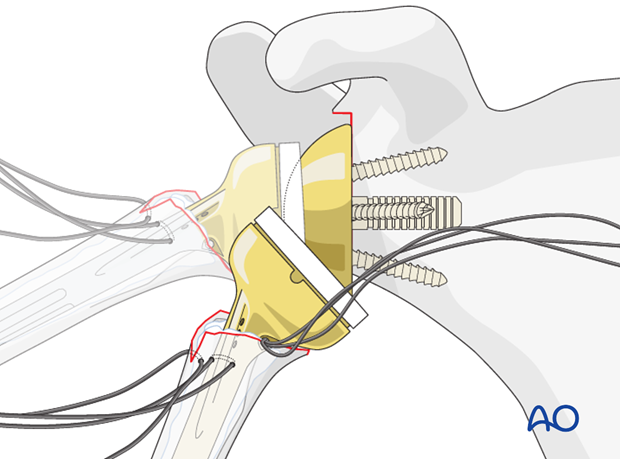
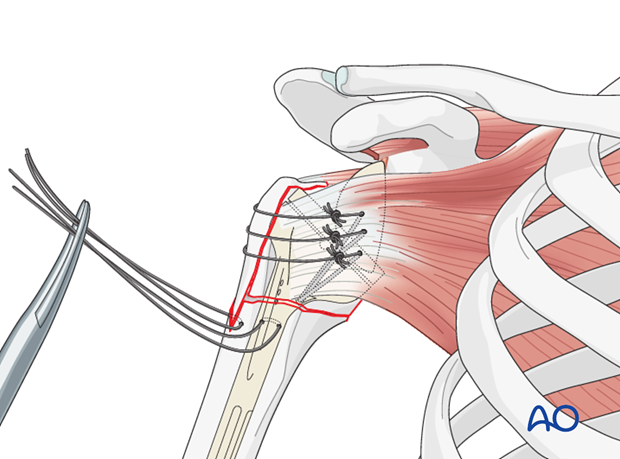
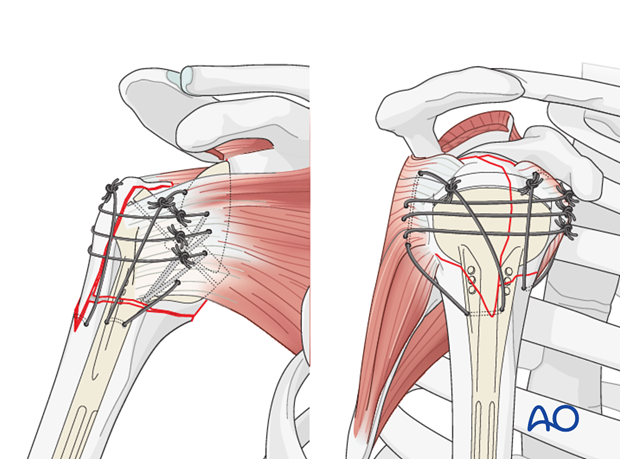
9. Fixation of the tuberosities