Tibial Plateau Fractures: Anatomy, Diagnosis, and Treatment
Tibial Plateau Fractures: Anatomy, Diagnosis, and Treatment
Tibial Plateau Fractures: Anatomy, Diagnosis, and Treatment
Tibial plateau fractures are periarticular injuries of the proximal tibia frequently associated with soft tissue injury. This article provides an overview of the anatomy, epidemiology, etiology, presentation, diagnosis, treatment, potential complications, and prognosis of tibial plateau fractures:
Mohammad Hutaif (  ORCID ID: 0009-0001-1092-5600) via Google Scholar.
ORCID ID: 0009-0001-1092-5600) via Google Scholar.
Save Cite Cited by Related articles All versions Import into BibTeX
Summary
Tibial plateau fractures are typically diagnosed with knee radiographs but frequently require CT scan for surgical planning. Treatment often involves ORIF in the acute setting versus delayed fixation after soft tissue swelling subsides.
Epidemiology
Incidence: Tibial plateau fractures occur in 1-2% of all fractures and have an incidence of 10.3 per 100,000 people annually.
Demographics: Tibial plateau fractures occur most commonly in males in their 40s due to high-energy trauma and females in their 70s due to low-energy falls. The lateral plateau is affected in 70-80% of cases, while bicondylar and medial plateau fractures account for 10-30% and 10-20%, respectively.
Etiology
Mechanism: Tibial plateau fractures are caused by the vector of applied load, amount of energy, and quality of bone. Valgus load causes lateral plateau fractures, while varus load causes medial plateau fractures. Axial load causes bicondylar fractures, and combination fractures can also occur. Fracture dislocation is associated with high-energy trauma and typically involves the medial-sided plateau.
Associated conditions: Meniscal tears, ACL injuries, compartment syndrome, and neurovascular injury can all be associated with tibial plateau fractures. Soft tissue injury is frequently seen with these fractures and can impact surgical planning and outcomes.
Anatomy
Figure 1: Tibial Plateau Fractures (Source: Hutaif Orthopedic Center)
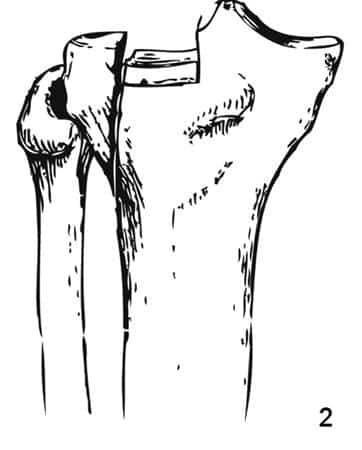
Osteology: The proximal tibia is divided into the lateral and medial tibial plateau. The lateral tibial plateau is convex in shape, while the medial tibial plateau is concave. The posterior tibial slope is 6-10°, and the varus slope is 3° relative to the mechanical axis of the tibia.
Figure 2: Alignment of Proximal Tibia (Source: Hutaif Orthopedic Center)
Ligaments: The knee joint is stabilized by several ligaments, including the ACL, PCL, MCL, and LCL. The menisci also play a role in knee stabilization.
Figure 3: Ligaments (Source: Hutaif Orthopedic Center)
Classification
Schatzker classification: This classification system categorizes tibial plateau fractures into six types based on the pattern of the fracture. Type I is a lateral split fracture, Type II is a lateral split-depressed fracture, Type III is a lateral pure depression fracture, Type IV is a medial plateau fracture, Type V is a bicondylar fracture, and Type VI is a metaphyseal-diaphyseal disassociation.
Figure 4: Schatzker Classification (Source: Hutaif Orthopedic Center)
3-column concept: This concept divides the tibial plateau into three columns: medial, lateral, and posterior. This helps to determine fixation strategy and includes posterior plateau fractures that are not considered in the Schatzker classification.
Figure 5: 3-Column Concept (Source: Hutaif Orthopedic Center)
Presentation
History: The mechanism of injury, functional status, and comorbidities should be assessed.
Physical exam: Examine for pain, tenderness, and swelling. Assess for any laxity on varus/valgus stress testing or instability in full extension. Evaluate for neurovascular injury and compartment syndrome.
Diagnosis and Treatment
MCQ 2
What is the most common type of tibial plateau fracture?
Discussion
The correct answer is Lateral split-depressed fracture. This is the most common type of tibial plateau fracture.
MCQ 3
Which ligaments are primary stabilizers of the knee joint?
Discussion
The correct answer is ACL and MCL. These ligaments are the primary stabilizers of the knee joint.
MCQ 4
What is the goal of treatment for tibial plateau fractures?
Discussion
The goal of treatment for tibial plateau fractures is to restore alignment and congruent articular surface.
MCQ 5
What is the most common complication associated with tibial plateau fractures?
Discussion
The most common complication associated with tibial plateau fractures is post-traumatic arthritis.
MCQ 6
What is the most common type of tibial plateau fracture in females?
Discussion
The most common type of tibial plateau fracture in females is Bicondylar fracture.