Mastering Radiology: Interactive Questions on Perilunate Dislocation
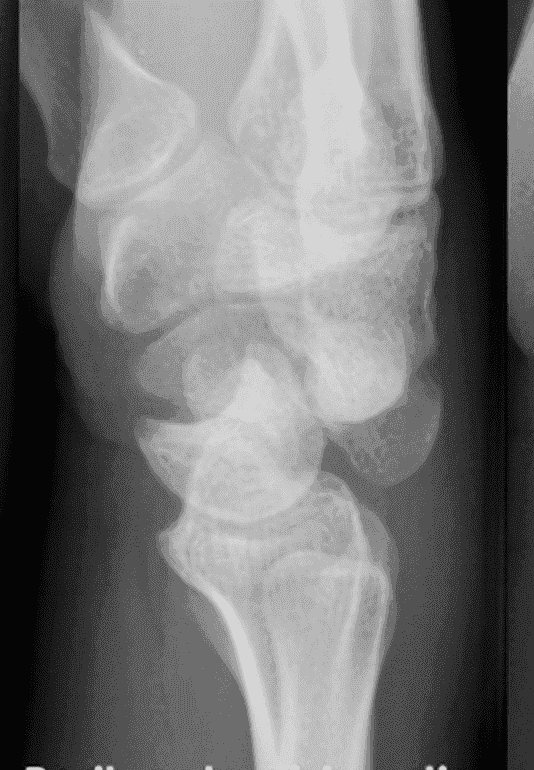
Peri-lunate dislocation
The image shows dorsal dislocation of the capitate which should be congruous with the cup of the lunate
Click here to see more
Perilunate Dislocations and Fracture-Dislocations
The lunate, which is normally securely attached to the distal radius by ligamentous attachments, is commonly referred to as the “carpal keystone.”
GREATER ARC INJURY
Greater arc injury passes through the scaphoid, capitate, triquetrum, or distal radial styloid and often results in transscaphoid, transcapitate, or transradial styloid perilunate fracture-dislocations.
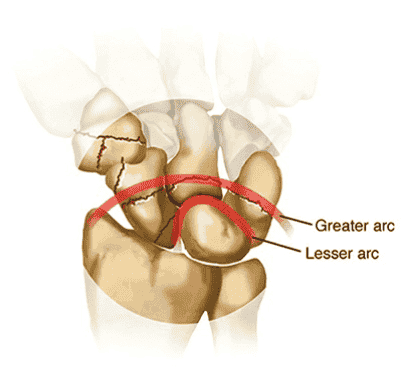
LESSER ARC INJURY
Lesser arc injury follows a curved path around the lunate, involving only the capsuloligamentous tissues through the scapholunate ligament, midcarpal joint, and lunotriquetral ligaments and results in perilunate and lunate dislocations. The most common injury is transscaphoid perilunate fracture-dislocation. Disruption of the normal kinematics and stability of the carpal row lead to acute failure with a predictable pattern of posttraumatic changes.
MECHANISM OF INJURY
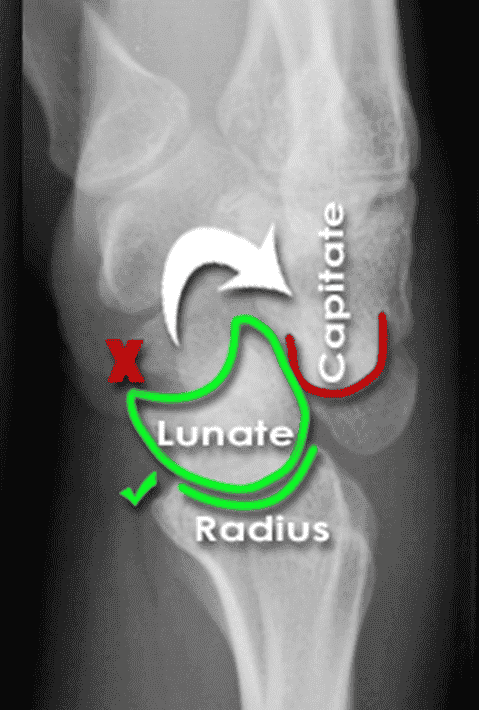
Perilunate injuries: Axial load is applied to the thenar eminence, forcing the wrist into extension. Injury progresses through several stages (Mayfield progression): It usually begins radially through the body of scaphoid (fracture) or through scapholunate interval (dissociation), although both are possible in the same injury (rare). Force is then transmitted ulnarly through the space of Poirier (between the lunate and capitate). Subsequently, force transmission disrupts the lunotriquetral articulation. This results in dorsal dislocation of the capitate and rest of the carpus relative to the lunate. Finally, the lunate can dislocate volarly out of the lunate fossa of the distal radius, in which case it is called the lunate dislocation. In a lunate dislocation, the proximal part of the capitate sits in the lunate fossa.
CLINICAL EVALUATION
Scapholunate or perilunate injuries typically cause tenderness just distal to Lister tubercle. Swelling is generalized about the wrist with variable dorsal prominence of the entire carpus in cases of dorsal perilunate dislocations.
RADIOGRAPHIC EVALUATION
PA, lateral, and oblique views should be obtained to confirm the diagnosis and rule out associated injuries. A CT scan may be useful in further defining the injury pattern.
PA View
The dislocated lunate appears to be wedge-shaped and more triangular, with an elongated volar lip. Loss of normal carpal colinear “Gilula lines” and abnormal widening of the scapholunate interval >3 mm are noted. Look for associated fractures, such as “transscaphoid” injuries.

Lateral View
Most important view. Carefully look at the outline of the capitate and lunate. The “spilled teacup sign” occurs with volar dislocation of the lunate. A clenched-fist PA view obtained after closed reduction of the midcarpal joint is useful for checking residual scapholunate or lunotriquetral dissociation as well as fractures.
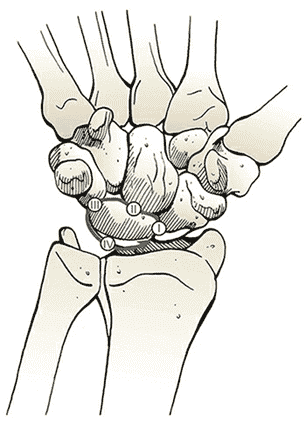
CLASSIFICATION (MAYFIELD)
| Stage | Description |
|---|---|
| Stage I | Disruption of the scapholunate joint: The radioscapholunate and interosseous scapholunate ligaments are disrupted. |
| Stage II | Disruption of the midcarpal (capitolunate) joint: The radioscaphocapitate ligament is disrupted. |
| Stage III | Disruption of the lunotriquetral joint: The distal limb of the radiolunotriquetral ligament and the ulnotriquetrocapitate complex is disrupted. |
| Stage IV | Disruption of the radiolunate joint: The dorsal radiolunotriquetral ligament is disrupted, ultimately causing volar dislocation of the lunate. |
TREATMENT
Closed reduction should be performed with adequate sedation. Closed reduction of lunate dislocations is frequently unsuccessful. Early surgical reconstruction is performed if swelling allows. Immediate surgery including open carpal tunnel release is needed if there are progressive signs of median nerve compromise. Most transscaphoid perilunate dislocations are best treated by open volar and dorsal reduction and repair of the injured structures. Open repair should be supplemented by pin fixation while ligaments heal. Delayed reconstruction is indicated if early intervention is not feasible.
COMPLICATIONS
Median neuropathy may result from carpal tunnel compression, necessitating surgical release. Posttraumatic arthritis may result from the initial injury or secondarily from small, retained osseous fragments and cartilage damage. Chronic perilunate injury may result from untreated or inadequately treated dislocation or fracture-dislocation resulting in chronic pain, instability, and wrist deformity, often associated with tendon rupture or increasing nerve symptoms. Recurrent instability may necessitate ligament reconstruction with capsular augmentation. If recurrent instability persists, lunotriquetral fusion may be necessary, with possible concomitant ulnar shortening to tension the volar ulnocarpal ligaments.

