Orthopedic MD Oral Examination:Management of Proximal Humerus Fracture
Varus Proximal Humerus Fracture
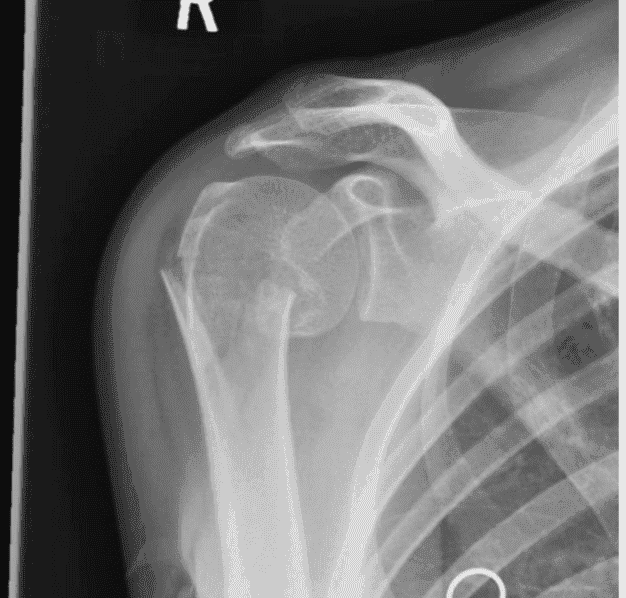
This is an AP radiograph of the right shoulder demonstrating a two-part, varus displaced, surgical neck of humerus fracture.
Click here to see more
Proximal Humerus Fractures
EPIDEMIOLOGY
| Constitutes | 4% to 5% of all fractures | Incidence is 300,000 per year (more common than hip fracture) | Most (85%) are nondisplaced |
| Older individuals | Higher incidence secondary to osteoporosis | A proximal humerus fracture in an older individual after a simple fall is considered a fragility fracture | The 2:1 female-to-male ratio is also related to osteoporosis |
ANATOMY
- The shoulder has the greatest range of motion of any joint in the body, secondary to the shallow glenoid fossa that is only 25% the size of the humeral head. The major contributor to stability is not bone but the soft tissue envelope composed of muscle, capsule, and ligaments.
- The proximal humerus is retroverted 35 to 40 degrees relative to the epicondylar axis.
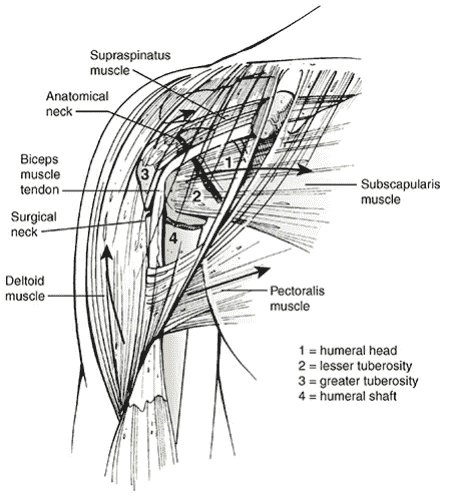
- The shoulder has four osseous segments (Neer): humeral head, lesser tuberosity, greater tuberosity, and humeral shaft.
Deforming muscular forces on the proximal humerus:
- The supraspinatus and external rotators, which displace the greater tuberosity superior and posterior
- The subscapularis, which displaces the lesser tuberosity medially
- The pectoralis major, which displaces the humeral shaft medially
- The deltoid, which abducts the proximal fragment
Neurovascular supply
- The major blood supply is from the anterior and posterior humeral circumflex arteries.
- The axillary nerve courses just anteroinferior to the glenohumeral joint, traversing the quadrangular space. It is at particular risk for traction injury owing to its relative rigid fixation at the posterior cord and deltoid as well as its proximity to the inferior capsule where it is susceptible to injury during anterior dislocation and anterior fracture-dislocation.
MECHANISM OF INJURY
The most common mechanism is a fall onto an outstretched upper extremity from a standing height, typically in an older woman (fragility fracture). Younger patients typically sustain a proximal humeral fracture following high-energy trauma, such as a motor vehicle accident. These usually represent more severe fractures and dislocations, with significant associated soft tissue disruption and multiple injuries. Less common mechanisms include excessive shoulder abduction in an individual with osteoporosis, in which the greater tuberosity prevents further rotation; direct trauma, usually associated with greater tuberosity fractures; electrical shock or seizure (associated with dislocation); and pathologic processes, such as malignant or benign processes in the proximal humerus.
CLINICAL EVALUATION
- Patients typically present with the arm held closely to the chest by the contralateral hand, with shoulder pain, swelling, tenderness, painful range of motion, and variable crepitus.
- A careful neurovascular examination is essential, with particular attention to axillary nerve function.
RADIOGRAPHIC EVALUATION
A shoulder series, consisting of an anteroposterior and lateral (“Y”) views in the scapular plane as well as an axillary, is standard. Computed tomography is helpful in evaluating articular involvement, degree of fracture displacement, impression fractures, and glenoid rim fractures. Magnetic resonance imaging is generally not indicated for fracture management, but it may be used to assess rotator cuff integrity.
CLASSIFICATION
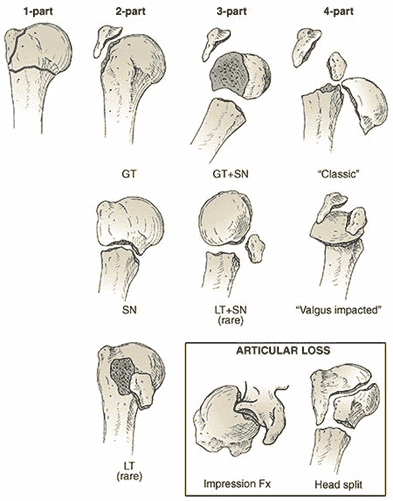
Neer
Defines four parts: These are the greater and lesser tuberosities, humeral shaft, and humeral head. A part is defined as displaced if >1 cm of fracture displacement or >45 degrees of angulation. Fracture types:
| Fracture Type | Description |
|---|---|
| One-part fractures | No displaced fragments regardless of number of fracture lines |
| Two-part fractures |
|
| Three-part fractures |
|
| Four-part fractures |
|
Orthopaedic Trauma Association
See Fracture and Dislocation Compendium at: https://ota.org/research/fracture-and-dislocation-compendium
TREATMENT
Minimally displaced fractures (one-part fracture)
- Sling immobilization or swathe for comfort
- Early shoulder motion at 7 to 10 days consisting of pendulum exercises and passive range of motion
- Early radiographic follow-up to detect loss of fracture reduction
- Active range-of-motion exercises are started 6 weeks after injury
- Resistive exercises are started anywhere from 6 to 12 weeks
- Return to near full range of motion and function is the expected outcome by 1 year
Two-part fractures - anatomic neck fractures
Rare and difficult to treat by closed reduction. They require open reduction and internal fixation (ORIF) (younger patients) or prosthetic replacement (older individuals) and have been historically associated with a higher incidence of osteonecrosis.
Two-part fractures - surgical neck fractures
- Nonoperative treatment is rarely indicated except for angulated/displaced surgical neck fractures, which are stable (move as a unit) in lower demand individuals, severely debilitated patients, and those who cannot tolerate surgery.
- Closed reduction and percutaneously inserted terminally threaded pins or cannulated screws may be considered in younger individuals with good-quality bone. Problems associated with multiple pin fixation include nerve injury (axillary), pin loosening, pin migration, and inability to move the arm.
- ORIF is the treatment of choice for most displaced surgical neck fractures of the proximal humerus and can involve placement of plate and screws or an intramedullary device. Most current proximal humerus plates use a locked screw construct for the metaphyseal component secondary to improved fixation of locked screws in osteopenic cancellous bone.
- Prosthetic replacement may be considered for patients with extreme osteopenia and involves use of hemiarthroplasty, total shoulder, or reverse shoulder prosthesis.
Two-part fractures - greater tuberosity fractures
ORIF with or without rotator cuff repair is indicated for greater tuberosity fractures which are displaced >5 to 10 mm (5 mm for superior translation); otherwise, they may develop nonunion and subacromial impingement. A greater tuberosity fracture associated with anterior dislocation may reduce on reduction of the glenohumeral joint and be treated nonoperatively.
Two-part fractures - lesser tuberosity fractures
They may be treated closed unless displaced fragment blocks internal rotation; one must rule out associated posterior dislocation.
Three-part fractures
- Usually unstable due to opposing muscle forces; as a result, closed reduction and maintenance of reduction are often difficult.
- Displaced fractures require operative treatment, except in severely debilitated patients or those who cannot tolerate surgery.
- Younger individuals should have an attempt at ORIF using plate and screws; preservation of the vascular supply is of paramount importance with minimization of soft tissue devascularization.
- Locking plate technology has expanded the indications for ORIF after three-part fracture in older individuals, secondary to improved screw fixation in osteopenic bone. However, one should be prepared to perform prosthetic replacement (hemiarthroplasty, total shoulder, or reverse shoulder prosthesis) in older individuals if necessary. There has been increased use of reverse shoulder prostheses as a prosthetic replacement after proximal humerus fractures in the elderly because of difficulty with tuberosity attachment and healing with conventional hemiarthroplasty.
Four-part fractures
- Incidence of osteonecrosis ranges from 4% to 35%.
- ORIF may be attempted in patients with good-quality bone if the humeral head is located within the glenoid fossa and there appears to be soft tissue continuity. Fixation is best achieved with locking plate and screw fixation, suture, and/or wire fixation.
- Primary prosthetic replacement of the humeral head (reverse shoulder prosthesis) is indicated in the elderly.
- Hemiarthroplasty is associated with predictable pain relief but with unpredictable results from the standpoint of function; has fallen out of favor in older individuals.
- Reverse total shoulder arthroplasty (rTSA) has demonstrated results similar to successful ORIF and better than hemiarthroplasty for fracture; has unique set of complications associated.
Fracture-dislocations
- Two-part fracture-dislocations: may be treated closed after shoulder reduction unless the fracture fragments remain displaced.
- Three- and four-part fracture-dislocations: ORIF is used in younger individuals and prosthetic replacement in the elderly depending on the length of dislocation. The brachial plexus and axillary artery are in proximity to the humeral head fragment with anterior fracture-dislocations.
- Recurrent dislocation is rare following fracture union.
- Prosthetic replacement for anatomic neck fracture-dislocation is recommended because of the high incidence of osteonecrosis.
- These injuries may be associated with increased incidence of myositis ossificans with repeated attempts at closed reduction.
SURGICAL CONSIDERATIONS
Patient positioning
Supine or beach chair position. The supine position is easier to set up and bring in fluoroscopy. The beach chair position allows the weight of the arm to facilitate fracture reduction. In addition, prosthetic replacement is usually performed in a beach chair position.
Surgical approach
Deltopectoral versus deltoid split. The deltopectoral approach is the workhorse of the shoulder and allows for an extensile approach to the proximal humerus. ORIF or arthroplasty is well performed through this approach. The deltoid split allows for easier plate placement on the greater tuberosity and requires fewer assistants to retract the deltoid muscle.
COMPLICATIONS
- Vascular injury: This is infrequent (5% to 6%), the axillary artery is the most common site (proximal to anterior circumflex artery). The incidence is increased in older individuals with atherosclerosis because of the loss of vessel wall elasticity. There is a rich collateral circulation about the shoulder, which could mask vascular injury.
- Neural injury
- Brachial plexus injury: This is infrequent (6%).
- Axillary nerve injury: This is particularly vulnerable with anterior fracture-dislocation because the nerve courses on the inferior capsule and is prone to traction injury or laceration. Complete axillary nerve injuries that do not improve within 2 to 3 months may require electromyographic evaluation and exploration.
- Chest injury: Intrathoracic dislocation may occur with surgical neck fracture-dislocations; pneumothorax and hemothorax must be ruled out in the appropriate clinical setting.
- Myositis ossificans/heterotopic ossification: This is uncommon and is associated with chronic unreduced fracture-dislocations and repeated attempts at closed reduction. It may also be related to timing of surgery and deltoid split approaches.
- Shoulder stiffness: It may be minimized with an aggressive, supervised physical therapy regimen and may require open lysis of adhesions for recalcitrant cases.
- Osteonecrosis: This may complicate 3% to 14% of three-part proximal humeral fractures, 4% to 34% of four-part fractures, and a high rate of anatomic neck fractures.
- Nonunion: This occurs particularly in displaced two-part surgical neck fractures with soft tissue interposition. Other causes include excessive traction, severe fracture displacement, systemic disease, poor bone quality, inadequate fixation, and infection. It may be addressed with ORIF with or without bone graft or prosthetic replacement.
- Malunion: This occurs after inadequate closed reduction or failed ORIF and may result in impingement of the greater tuberosity on the acromion, with subsequent restriction of shoulder motion. It is important to restore medial cortical support by either anatomic fracture reduction, use of oblique inferomedial locking screws, or an allograft strut to prevent varus collapse.
Click here to see more
Proximal Humerus Fractures
SUMMARY
Proximal humerus fractures are common fractures often seen in older patients with osteoporotic bone following a ground-level fall on an outstretched arm. Diagnosis is made with orthogonal radiographs of the shoulder. Treatment with sling immobilization is indicated for minimally displaced fractures with surgical fixation versus arthroplasty indicated in more complex and displaced fractures.
EPIDEMIOLOGY
- Incidence: common; 4-6% of all fractures
- Demographics:
- 2:1 female to male ratio
- Increasing age associated with more complex fracture types
- Anatomic location: may occur at the surgical neck, anatomic neck, greater tuberosity, and lesser tuberosity; two-part surgical neck fractures are most common
- Risk factors:
- Osteoporosis
- Diabetes
- Epilepsy
- Female gender
ANATOMY
Osteology
- Anatomic neck represents the old epiphyseal plate; surgical neck represents the weakened area below head; more often involved in fractures than anatomic neck; average neck-shaft angle is 135 degrees
Muscles
- Pectoralis major displaces shaft anteriorly and medially
- Supraspinatus, infraspinatus, and teres minor externally rotate greater tuberosity
- Subscapularis internally rotates articular segment or lesser tuberosity
Ligaments
- Coracohumeral ligament attaches to coracoid and greater tuberosity and strengthens the rotator interval
- SGHL restraint to inferior translation at 0° degrees of abduction (neutral rotation)
- MGHL resists AP translation in the midrange (~45°) of abduction
- IGHL restraint to AP translation at 90° degrees of abduction
Blood Supply
- Anterior humeral circumflex artery with large number of anastomosis with other vessels in the proximal humerus
- Branches:
- Anterolateral ascending branch; arcuate artery is the terminal branch and main supply to greater tuberosity
- Posterior humeral circumflex artery; recent studies suggest it is the main blood supply to humeral head
CLASSIFICATION
AO/OTA
Organizes fractures into 3 main groups and additional subgroups based on fracture location, status of the surgical neck, and presence/absence of dislocation.
Neer classification
Based on anatomic relationship of 4 segments: greater tuberosity, lesser tuberosity, articular surface, and shaft. Considered a separate part if displacement of > 1 cm or 45° angulation.
Minimally displaced, two-part, three-part, four-part, anatomical neck, surgical neck, greater tuberosity, lesser tuberosity, fracture-dislocation, and head split.
PRESENTATION
Symptoms
- Pain and swelling
- Decreased motion
Physical exam
- Inspection: extensive ecchymosis of chest, arm, and forearm
- Neurovascular exam: axillary nerve injury most common; determine function of deltoid muscle and lateral shoulder sensation; arterial injury may be masked by extensive collateral circulation preserving distal pulses
- Examine for concomitant chest wall injuries
IMAGING
Radiographs
Recommended views: complete trauma series, true AP (Grashey), scapular Y, and axillary. Additional views include apical oblique, Velpeau, and West Point axillary. Findings may include combined cortical thickness (medial + lateral thickness >4 mm) and pseudosubluxation (inferior humeral head subluxation caused by blood in the capsule and muscular atony).
CT scan
- Indications: preoperative planning; humeral head or greater tuberosity position uncertain; intra-articular comminution; concern for head-split fracture
MRI
- Indications: rarely indicated; useful to identify associated rotator cuff injury
TREATMENT
Nonoperative
Sling immobilization followed by progressive rehabilitation.
- Indications: most proximal humerus fractures can be treated nonoperatively, including minimally displaced surgical and anatomic neck fractures and greater tuberosity fracture displaced < 5mm; fractures in patients who are not surgical candidates; additional variables to consider include age, fracture type, fracture displacement, bone quality, dominance, general medical condition, and concurrent injuries
- Outcomes: immediate physical therapy results in faster recovery
Operative
- CRPP (closed reduction percutaneous pinning)
- Indications: two-part surgical neck fractures; 3-part and valgus-impacted 4-part fractures in patients with good bone quality, minimal metaphyseal comminution, and intact medial calcar
- Outcomes: considerably higher complication rate compared to ORIF, HA, and RSA; axillary nerve at risk with lateral pins; musculocutaneous nerve, cephalic vein, and bicep tendon at risk with anterior pins
- ORIF
- Indications: greater tuberosity displaced > 5mm; displaced 2-part fractures; 3- and 4-part fractures in younger patients; head-splitting fractures in younger patients
- Outcomes: medial support necessary for fractures with posteromedial comminution; calcar screw placement critical to decrease varus collapse of head
- Intramedullary nailing
- Indications: surgical neck fractures or 3-part greater tuberosity fractures in younger patients; combined proximal humerus and humeral shaft fractures
- Outcomes: biomechanically inferior with torsional stress compared to plates; favorable rates of fracture healing and ROM compared to ORIF
- Arthroplasty
- Indications:
- Hemiarthroplasty: younger patients (40-65 years old) with complex fracture-dislocations or head-splitting components that may fail fixation; recommended use of convertible stems to permit easier conversion to RSA if necessary in future
- Reverse total shoulder: low-demand elderly individuals with non-reconstructible tuberosities and poor bone stock; older patients with fracture-dislocation; reverse total shoulder arthroplasty following failed nonoperative management is associated with better functional outcomes than reverse total shoulder arthroplasty following failed open reduction and internal fixation
- Outcomes: improved results if anatomic tuberosity reduction and healing, restoration of humeral height and version; poor results with tuberosity nonunion or malunion, retroversion of humeral component > 40°
- Indications:
COMPLICATIONS
- Screw cut-out: most common complication following periarticular locking plating fixation (up to 14%)
- Avascular necrosis: better tolerated than in lower extremity; no relationship to type of fixation (plate or cerclage wires)
- Nerve injury: axillary nerve injury most common (up to 58% with studies using EMG); increased risk with lateral (deltoid-splitting) approach; suprascapular nerve (up to 48%); musculocutaneous nerve at risk with anterior pin in CRPP
- Malunion: usually varus apex-anterior or malunion of GT; poor results if converting from varus malunited fracture to TSA; use reverse shoulder arthroplasty instead
- Nonunion: most common after two-part surgical neck fracture; treatment of chronic nonunion/malunion in the elderly should include arthroplasty; lesser tuberosity nonunion leads to weakness with lift-off testing; greater tuberosity nonunion after arthroplasty leads to lack of active shoulder elevation; greatest risk factors for nonunion are age and smoking
- Rotator cuff injuries and dysfunction: long head of biceps tendon injuries also at risk with anterior pin in CRPP; missed posterior dislocation; adhesive capsulitis and scar tissue; posttraumatic arthritis; infection



