Mastering the Management of Scaphoid Fractures: Understanding Classification, Treatment, and Complications
Scaphoid Fracture
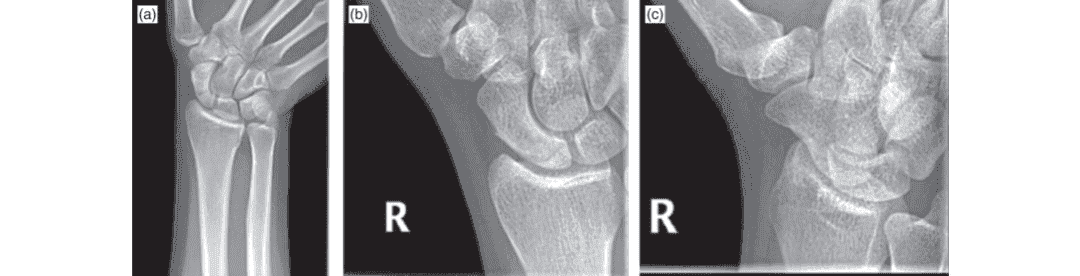
These scaphoid views demonstrate a fracture of the proximal pole of the scaphoid.
Click here to see more
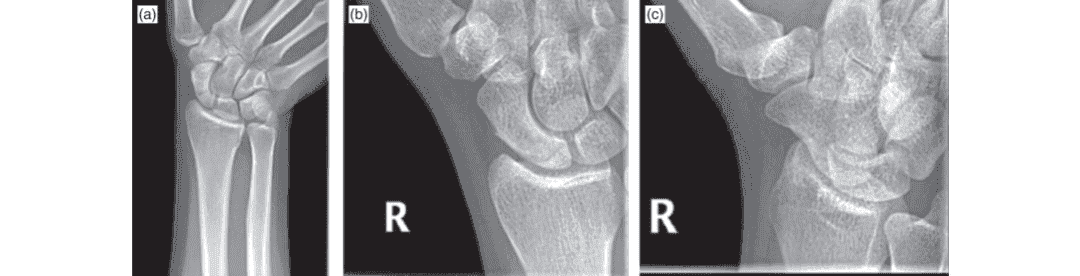
Scaphoid Fracture
These scaphoid views demonstrate a fracture of the proximal pole of the scaphoid.
Click here to see more
Scaphoid Fractures
SUMMARY
Scaphoid Fractures are the most common carpal bone fracture, often occurring after a fall onto an outstretched hand. Diagnosis can generally be made by dedicated radiographs but CT or MRI may be needed for confirmation. Treatment may require a prolonged period of cast immobilization, percutaneous surgical fixation, or open reduction and internal fixation.
EPIDEMIOLOGY
| Incidence | 15% of acute wrist injuries | 60% of all carpal fracture | 8 per 100,000 females, 38 per 100,000 males |
| Demographics | 2 :1 male : female | most common in third decade of life | |
| Anatomic location | percentage of fractures by scaphoid anatomic location | ||
| waist -65% | proximal third - 25% | distal third - 10% |
ETIOLOGY
Pathophysiology
- most common mechanism of injury is axial load across a hyper-dorsiflexed, pronated and ulnarly-deviated wrist
- common in contact sports
- transverse fracture patterns are considered more stable than vertically or obliquely oriented fractures
Associated conditions
- SNAC (Scaphoid Nonunion Advanced Collapse)
ANATOMY
Osteology
- complex 3-dimensional structure described as resembling a boat, skiff, and twisted peanut
- oriented obliquely from extremity's long-axis (implications for advanced imaging techniques)
- largest bone in proximal carpal row
- > 75% of scaphoid bone is covered by articular cartilage
- articulates with radius, lunate, trapezium, trapezoid, and capitate
Blood supply
- major blood supply is dorsal carpal branch (branch of the radial artery)
- enters scaphoid in a nonarticular ridge on the dorsal surface and supplies proximal 80% of scaphoid via retrograde blood flow
- minor blood supply from superficial palmar arch (branch of volar radial artery)
- enters distal tubercle and supplies distal 20% of scaphoid
- creates vascular watershed and poor fracture healing environment
Biomechanics
link between proximal and distal carpal row; both intrinsic and extrinsic ligaments attach and surround the scaphoid; the scaphoid flexes with wrist flexion and radial deviation and extends during wrist extension and ulnar deviation (same as proximal row)
CLASSIFICATION
Herbert and Fisher Classification (based on fracture stability)
- Type A: Stable, acute fractures
- Type B: Unstable, acute fractures (distal oblique, complete waist, proximal pole, trans-scaphoid and perilunate associated fractures)
- Type C: Delayed union characterized by cyst formation and fracture widening
- Type D: Nonunion
Mayo classification (based on location of fracture line)
- Type I: Distal tubercle fracture
- Type II: Distal articular surface fracture
- Type III: Distal third fracture
- Type IV: Middle third fracture
- Type V: Proximal third fracture
Russe Classification (based on fracture pattern)
- Type I: Horizontal oblique fracture line
- Type II: Transverse fracture line
- Type III: Vertical oblique fracture line
PRESENTATION
History
- high or low energy fall onto outstretched hand
Symptoms
- variable level of pain over wrist
Physical exam
- inspection
- wrist swelling
- rarely any ecchymosis, hematoma, or gross deformity
- motion
- worsened wrist pain with circumduction
- pain with resisted pronation
- provocative tests
- anatomic snuffbox tenderness dorsally
- scaphoid tubercle tenderness volarly
- scaphoid compression test
- positive test when pain reproduced with axial load applied through thumb metacarpal
- 87-100% sensitivity and 74% specificity when all three tests positive within 24 hours of injury
IMAGING
Radiographs
- recommended views
- neutral rotation PA
- lateral
- semi-pronated (45°) oblique
- scaphoid
- 30 degree wrist extension, 20 degree ulnar deviation
- waist fractures seen best
- if radiographs are negative (27%) and there is a high clinical suspicion, repeat radiographs in 14-21 days
Bone scan
- indications: occult fractures in acute setting
- sensitivity and specificity: specificity of 98%, and sensitivity of 100%, PPV 85% to 93% when done at 72 hours
MRI
- indications: most sensitive for diagnosis of occult fractures < 24 hours; immediate identification of fractures / ligamentous injuries; assessment of vascular status of bone (vascularity of proximal pole)
- sensitivity and specificity: approach 100% for occult fractures
CT scan with 1mm cuts along scaphoid axis
- indications: best modality to evaluate fracture location, angulation, displacement, fragment size, extent of collapse, and progression of nonunion or union after surgery
- sensitivity and specificity: 62% sensitivity and 87% specific for determining stability and fracture; less effective than bone scan and MRI to diagnose occult fracture
TREATMENT
Nonoperative
- cast immobilization
- indications: stable nondisplaced fracture (majority of fractures); if patient has normal radiographs but there is a high level of suspicion can immobilize in thumb spica and reevaluate in 12 to 21 days
- outcomes: scaphoid fractures with <1mm displacement have union rate of 90%
Operative
- percutaneous screw fixation
- indications: unstable fractures as shown by proximal pole fractures, displacement > 1 mm without significant angulation or deformity, non-displaced waist fractures (to allow decreased time to union, faster return to work/sport, similar total costs compared to casting)
- outcomes: union rates of 90-95% with operative treatment of scaphoid fractures; CT scan is helpful for evaluation of union
- open reduction internal fixation
- indications: significantly displaced fracture patterns, 15° scaphoid humpback deformity, radiolunate angle > 15° (DISI), intrascaphoid angle of > 35°, scaphoid fractures associated with perilunate dislocation, comminuted fractures, unstable vertical or oblique fractures
- outcomes: accuracy of reduction correlated with rate of union
COMPLICATIONS
- Scaphoid Nonunion
- incidence: 5-10% following immobilization, higher rates for proximal pole fractures
- risk factors: vertical oblique fracture pattern, displacement >1mm, advancing age, nicotine use
- treatment: vascularized or nonvascularid bone grafting procedures
- Osteonecrosis
- incidence: 13-50% of all scaphoid fractures, many studies showing 100% in proximal fifth fractures with immobilization
- Malunion
- flexion of distal fragment and extension of proximal fragment due to pull of scapholunate interosseous ligament creating shortened bone with humpback deformity
- Subchondral bone penetration with arthrosis due to prominent hardware
- incidence: seen following mini-open fixation techniques, incidence has decreased with use of fluoroscopy
- treatment: revision surgical fixation versus implant removal following union
- SNAC wrist (scaphoid nonunion advanced collapse)



