Below-Knee Amputation for Tumors of Distal Leg, Ankle, and Foot - Surgical Management
Learn about surgical management for below-knee amputation for tumors of the distal leg, ankle, and foot. Find information about indications, anatomy, imaging, surgical management, and postoperative care.
Background
Extensive tumors of the distal leg, ankle, and foot often require a below-knee amputation (BKA) as the primary form of surgical treatment. With such extensive tumors in these locations, attempts at limb salvage often leave patients with a limb with very limited function. Conversely, advances in prosthetic design and engineering allow for BKA amputees to be very active in a variety of activities, often more active than patients who have had limb-sparing procedures for similar tumors.
In general, we recommend BKAs for most high-grade and many low-grade sarcomas of the foot, especially when they occur in the plantar aspect. About 1% of bone sarcomas occur in the foot; these are usually treated with a BKA.

Anatomy
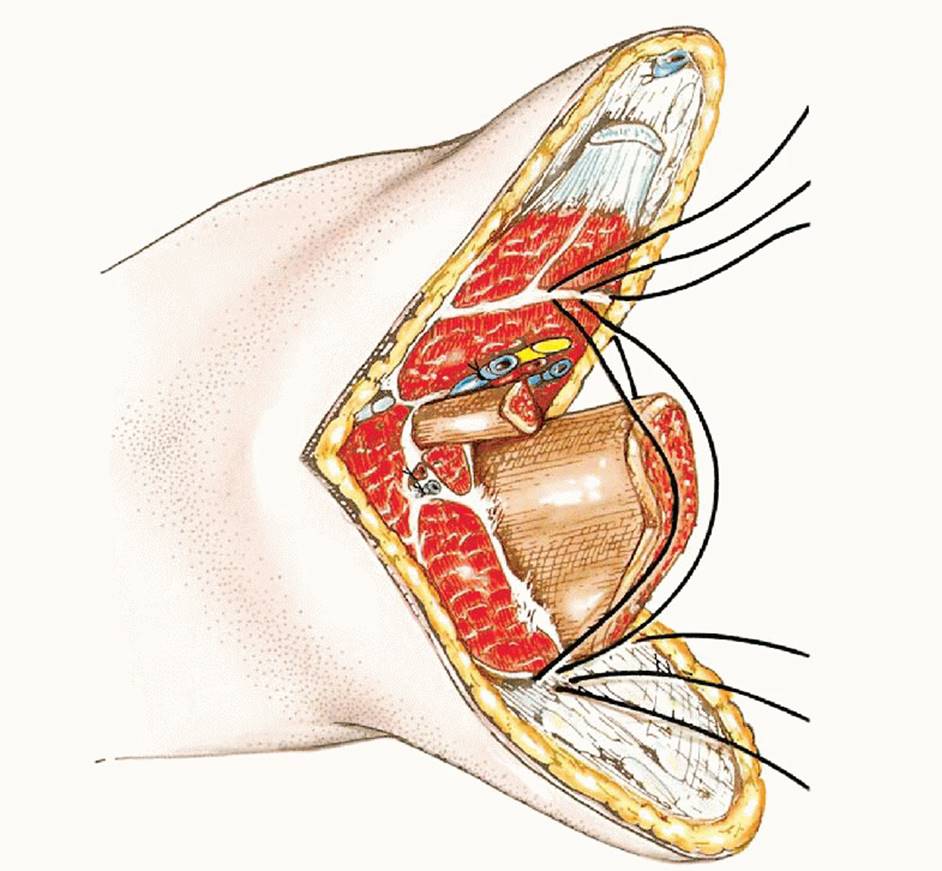
The main anatomic focus of a BKA is identification and ligation of the tibial neurovascular structures. The anterior tibial artery and vein and deep peroneal nerve lie deep to the anterior tibialis muscle and lateral to the tibia. These structures must be identified and individually ligated. As the dissection progresses posteriorly, the posterior tibial artery and vein and tibial nerve are found posterior to the tibia and tibialis posterior muscle and anterior to the soleus muscle. The peroneal artery and veins also lie posterior and lateral to the tibia. They lie between the tibialis posterior and the flexor hallucis longus. The superficial peroneal nerve is identified within the lateral compartment of the leg and also must be transected. It usually exits the fascia of the anterolateral leg approximately 12 cm proximal to the tip of the lateral malleolus. It should be identified and transected.
Indications
Tumor recurrence in the distal tibia, ankle, and foot not amenable to limb salvage techniques. Infiltrative high-grade soft-tissue sarcomas or other malignant tumors of the lower extremities. Extensive involvement of bone sarcomas of the lower extremities. Palliation. Failed attempt of radiation therapy for dorsal and plantar foot tumors.

Imaging and Other Staging Studies
Plain Radiography – Although plain radiographs are poor at identifying soft tissue tumors of the foot and ankle, they can be useful for the initial diagnosis of bone tumors such as enchondromas, giant cell tumors, and primary sarcomas of bone.
Computed Tomography and Magnetic Resonance Imaging – Computed tomography and magnetic resonance imaging (MRI) are helpful in determining the level of intramedullary tumor involvement and the extraosseous extent of the tumor, which is used to determine the amputation level. MRI is also useful for showing tumor involvement of neurovascular structures, which often necessitates amputation.
Bone Scanning – Bone scans are required if the tumor is located at or above the ankle. This study correlates well with the MRI. In general, amputation is performed 4 to 7 cm above abnormal findings on a bone scan.
Angiography and Other Studies – Angiography is very helpful in determining the extent of involvement of the anterior tibialis and posterior tibialis arteries. Tumor involvement of either of these structures determines the type of flap that should be used. This planning is important in minimizing wound healing problems.
Biopsy – As with an amputation at any level, a biopsy should be done to confirm the diagnosis before performing a BKA.
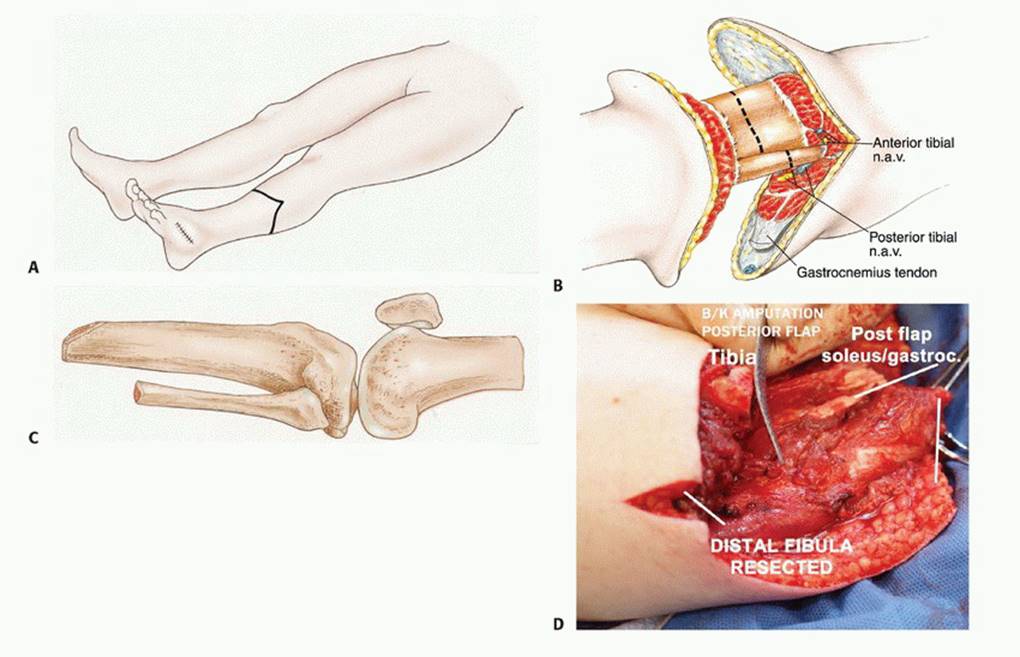
Surgical Management
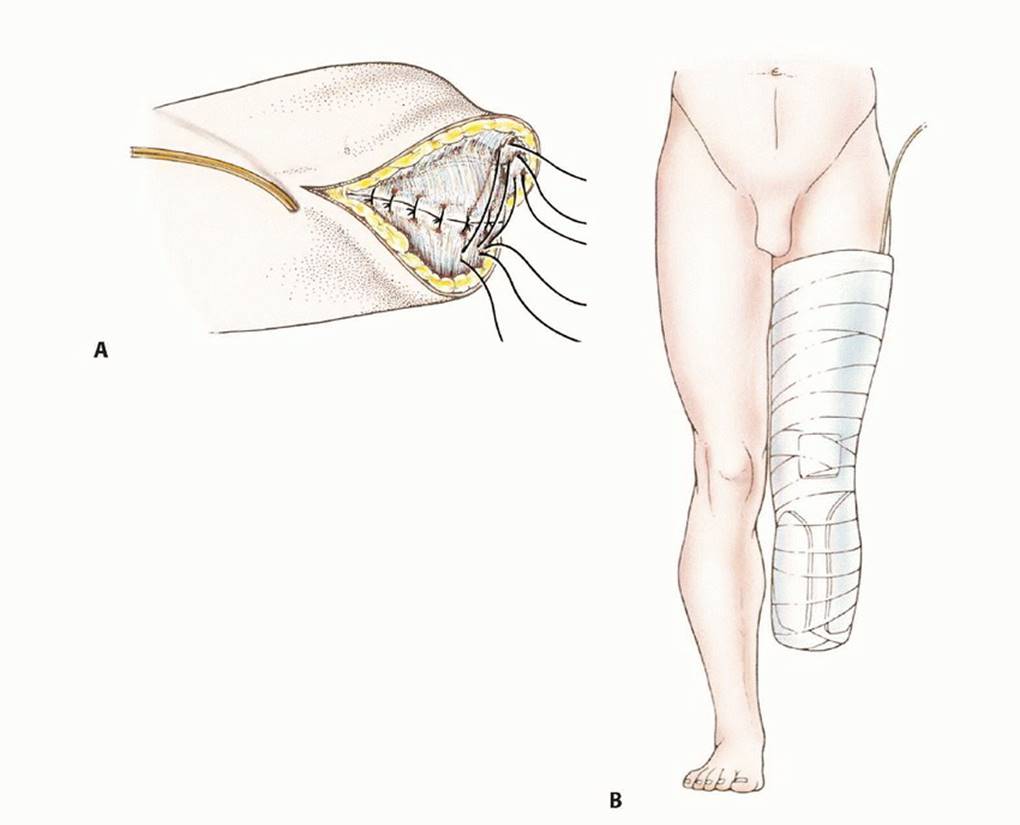
The ideal level of surgical resection for a BKA is at the musculocutaneous junction of the gastrocnemius muscle. This provides better soft tissue padding and usually a more reliable blood supply for the posterior flap. The recommended length for a BKA stump for optimal prosthetic fitting is 12.5 to 17.5 cm. However, tumor extent and margins will ultimately determine the length of the stump.
Careful flap selection is important in achieving a functional BKA stump. Because of the subcutaneous location of the tibia and sparse musculature of the anterior leg compartment, use of a long posterior flap is preferable to a fishmouth flap.
Prevention of hematoma and seroma development with the use of drains is critical. These complications can delay wound healing and, in some cases, delay adjunctive treatments such as chemotherapy and radiation therapy.
Postoperative Planning
Preoperative referrals to a psychologist and prosthetist are often useful in helping patients prepare for their upcoming life adjustments.
Positioning
The patient is supine on the operating table with the operative extremity slightly elevated.
Approach
The initial approach is made anteriorly in most cases. Then the knee can be flexed and abducted and adducted or an assistant can elevate the leg to gain exposure for the posterior work.
Postoperative Care
Once the initial postoperative dressing is removed, a stumpshrinker sock can be worn to minimize swelling. Patients should be counseled that the transition to prosthesis use will be slow and gradual and will occur over about 3 to 6 months. Once an initial prosthesis can be fitted, wear time is gradually increased to build tolerance.
p>
APA References
- Bahk WJ, et al. (2012). Effects of pneumatic tourniquet use on the outcomes of knee arthroscopy. Knee Surg Relat Res, 24(3): 153-9.
- National Academies of Sciences, Engineering, and Medicine. (2018). Public health consequences of e-cigarettes. National Academies Press.
- Al-Hassi HO, et al. (2021). Results of surgical treatment of shoulder instability in patients with Marfan syndrome. Hutaif Orthopedic Hospital Journal, 7(1): 21-26.
- Yamaguchi A, et al. (2014). Effectiveness of rehabilitation with Proprioceptive Neuromuscular Facilitation on ROM, strength and balance of the lower extremity after total knee arthroplasty. Oncology Letters, 8(5): 2089-2094.

