Below-Knee Amputation for Malignant Tumors of the Leg, Ankle, and Foot
Discover the indications, anatomy, imaging, and surgical management of below-knee amputation (BKA) for malignant tumors of the distal leg, ankle, and foot, as well as the postoperative care involved.
BACKGROUND
Extensive tumors of the distal leg, ankle, and foot often require a below-knee amputation (BKA) as the primary form of surgical treatment. With such extensive tumors in these locations, attempts at limb salvage often leave patients with a limb with very limited function. Conversely, advances in prosthetic design and engineering allow for BKA amputees to be very active in a variety of activities, often more active than patients who have had limb-sparing procedures for similar tumors.
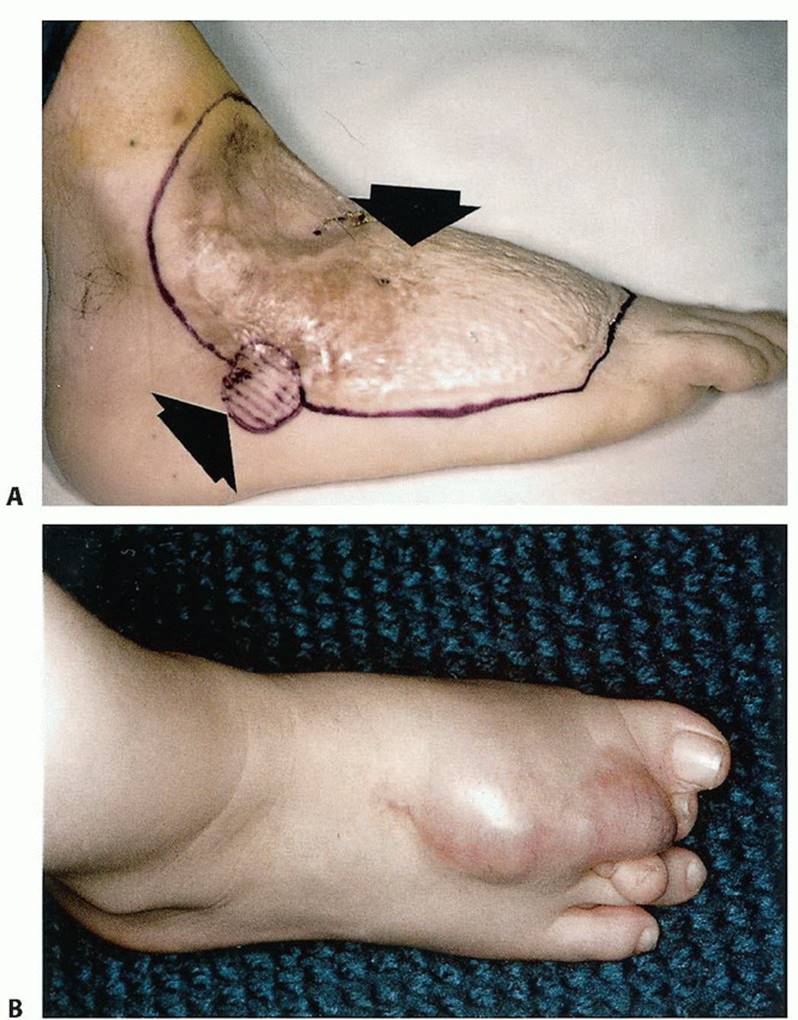
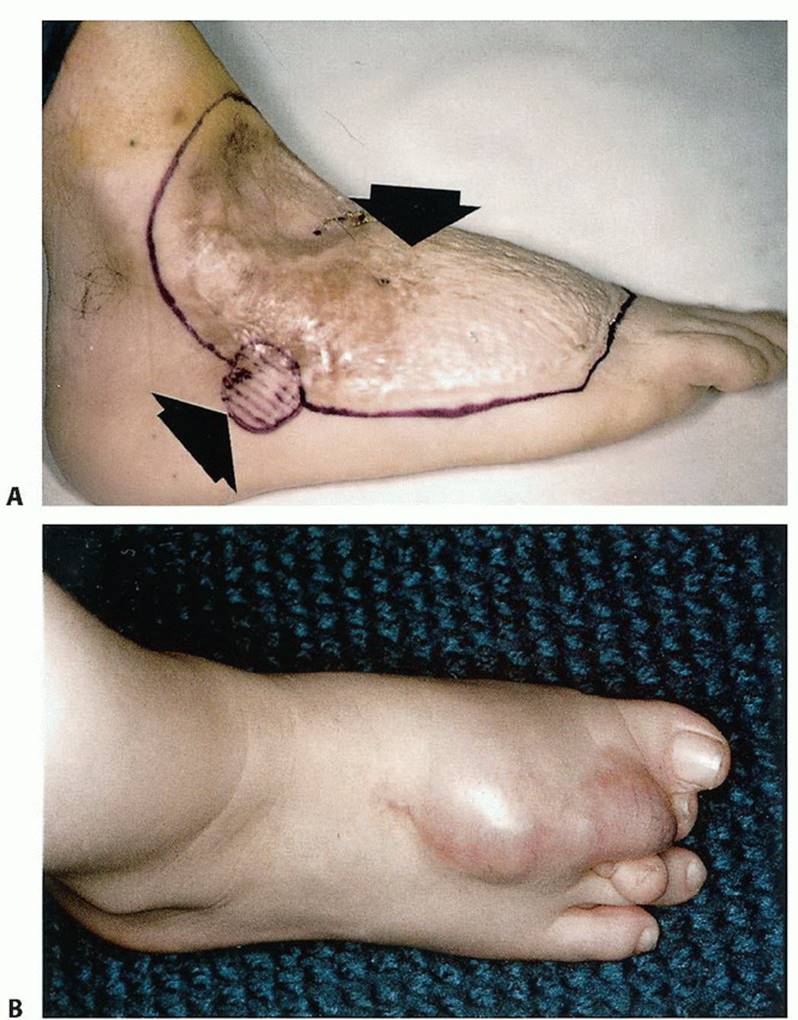
In general, we recommend BKAs for most high-grade and many low-grade sarcomas of the foot, especially when they occur in the plantar aspect. About 1% of bone sarcomas occur in the foot; these are usually treated with a BKA (FIG 1).

ANATOMY
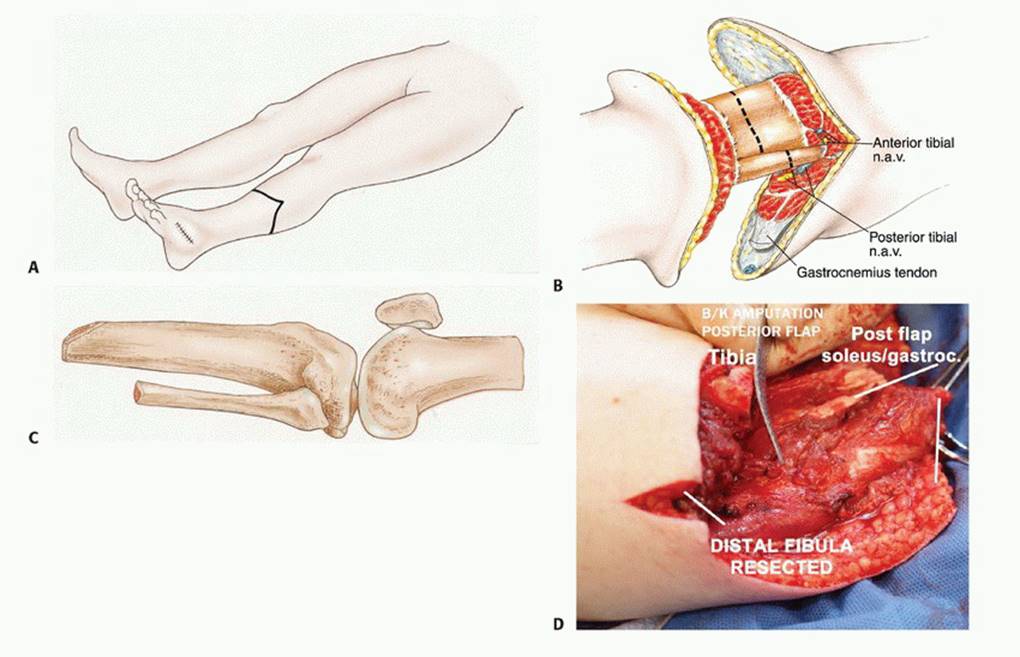
The main anatomic focus of a BKA is identification and ligation of the tibial neurovascular structures. The anterior tibial artery and vein and deep peroneal nerve lie deep to the anterior tibialis muscle and lateral to the tibia. These structures must be identified and individually ligated. As the dissection progresses posteriorly, the posterior tibial artery and vein and tibial nerve are found posterior to the tibia and tibialis posterior muscle and anterior to the soleus muscle. The peroneal artery and veins also lie posterior and lateral to the tibia. They lie between the tibialis posterior and the flexor hallucis longus. The superficial peroneal nerve is identified within the lateral compartment of the leg and also must be transected. It usually exits the fascia of the anterolateral leg approximately 12 cm proximal to the tip of the lateral malleolus. It should be identified and transected.
INDICATIONS
- Tumor recurrence in the distal tibia, ankle, and foot not amenable to limb salvage techniques (FIG 2)
- Infiltrative high-grade soft tissue sarcomas or other malignant tumors of the lower extremities
- Extensive involvement of bone sarcomas of the lower extremities
- Palliation
- Failed attempt of radiation therapy for dorsal and plantar foot tumors
IMAGING AND OTHER STAGING STUDIES
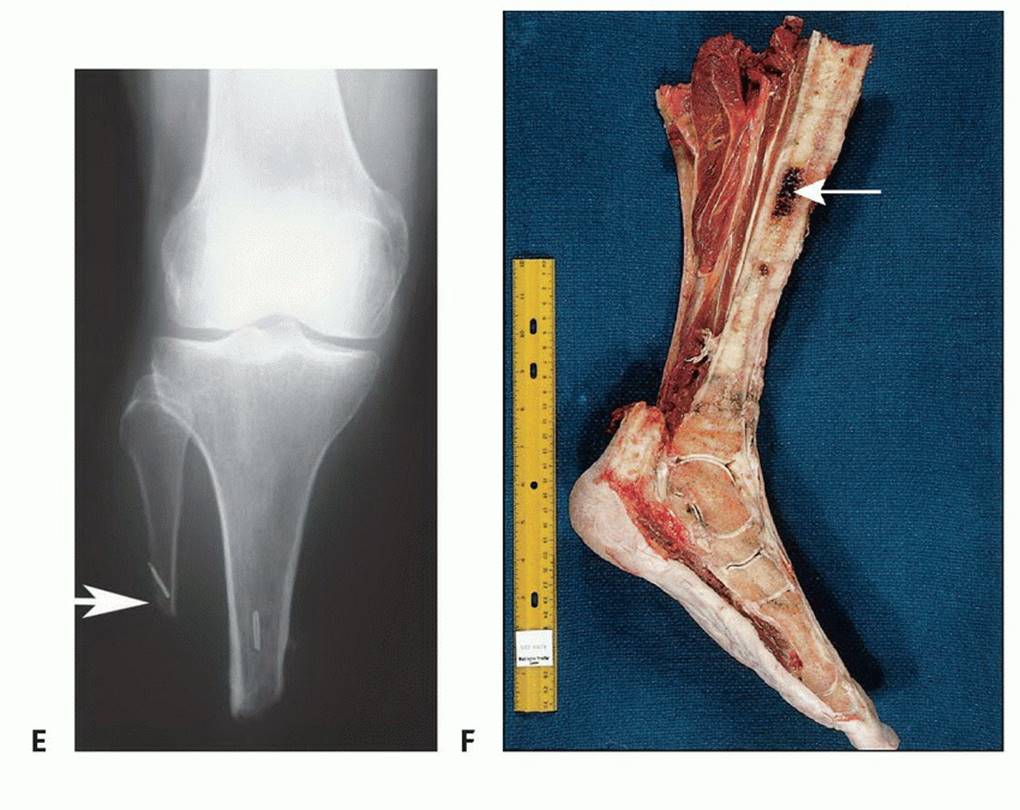
Plain Radiography
Although plain radiographs are poor at identifying soft tissue tumors of the foot and ankle, they can be useful for the initial diagnosis of bone tumors such as enchondromas, giant cell tumors, and primary sarcomas of bone (FIG 3A).

Computed Tomography and Magnetic Resonance Imaging
Computed tomography and magnetic resonance imaging (MRI) are helpful in determining the level of intramedullary tumor involvement and the extraosseous extent of the tumor, which is used to determine the amputation level. MRI is also useful for showing tumor involvement of neurovascular structures, which often necessitates amputation (FIG 3B).
Bone Scanning
Bone scans are required if the tumor is located at or above the ankle. This study correlates well with the MRI. In general, amputation is performed 4 to 7 cm above abnormal findings on a bone scan.
Angiography and Other Studies
Angiography is very helpful in determining the extent of involvement of the anterior tibialis and posterior tibialis arteries. Tumor involvement of either of these structures determines the type of flap that should be used. This planning is important in minimizing wound healing problems.
Biopsy
As with an amputation at any level, a biopsy should be done to confirm the diagnosis before performing a BKA.
SURGICAL MANAGEMENT
The ideal level of surgical resection for a BKA is at the musculocutaneous junction of the gastrocnemius muscle. This provides better soft tissue padding and usually a more reliable blood supply for the posterior flap. The recommended length for a BKA stump for optimal prosthetic fitting is 12.5 to 17.5 cm. However, tumor extent and margins will ultimately determine the length of the stump. Careful flap selection is important in achieving a functional BKA stump. Because of the subcutaneous location of the tibia and sparse musculature of the anterior leg compartment, use of a long posterior flap is preferable to a fishmouth flap. Prevention of hematoma and seroma development with the use of drains is critical. These complications can delay wound healing and, in some cases, delay adjunctive treatments such as chemotherapy and radiation therapy. (FIG 1, TECH FIG 1, FIG 2, TECH FIG 2, TECH FIG 3A)







Preoperative Planning
Preoperative referrals to a psychologist and prosthetist are often useful in helping patients prepare for their upcoming life adjustments.
Positioning
The patient is supine on the operating table with the operative extremity slightly elevated.
Approach
The initial approach is made anteriorly in most cases. Then the knee can be flexed and abducted and adducted or an assistant can elevate the leg to gain exposure for the posterior work.
TECHNIQUES
Incision and Flap Selection, Soft Tissue Dissection, and Bone Transection
Because of the subcutaneous location of the tibia and the minimal musculature of the anterior leg compartment, a long posterior flap is preferable to the classic fish-mouth flap. In the initial incision, the skin, superficial fascia, and subcutaneous tissue are cut perpendicular to the skin surface (TECH FIG 1A). The muscles of the anterior, lateral, and deep compartments of the leg are transected using the electrocautery to minimize bleeding. Vascular structures are ligated in continuity and divided. Major blood vessels are suture-ligated (TECH FIG 1B). Nerves are meticulously dissected and gently pulled 2 cm out of their surrounding muscle mass. They are doubly ligated with monofilament nonabsorbable suture. The large muscle groups are tapered so that they can be secured over the cut ends of the bone. If the amputation is performed for a primary bone sarcoma, intramedullary content from the edge of the stump should be sent for frozen section to verify that it is free of tumor. If the amputation is performed for a soft tissue sarcoma, soft tissues from the surgical margins should be assessed in a similar manner. After transection, the tibial edge is beveled (TECH FIG 1C,D).
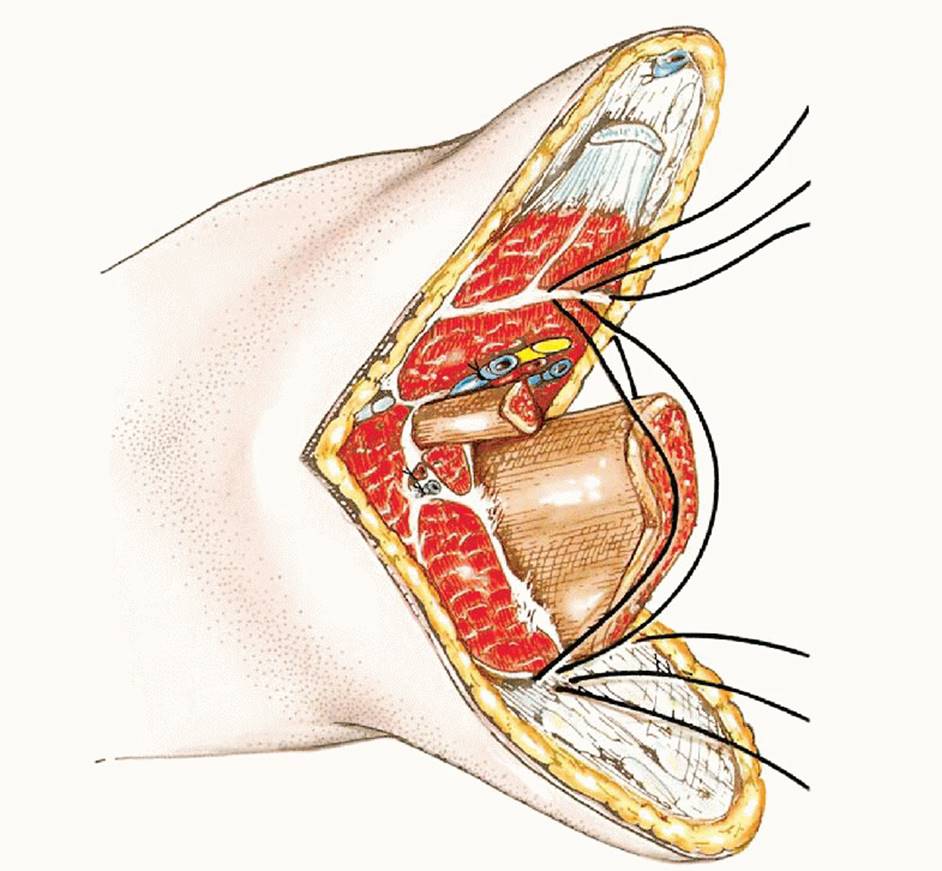

The tibia is osteotomized using an oscillating or Gigli saw. The fibula is resected several centimeters proximal to the tibial osteotomy to create a more tapered stump. The cut edge of the tibia is beveled using a saw or rasp to smooth the edges and contour the bone for a better prosthetic fit (TECH FIG 1E). A sample from the remaining intramedullary canal of the tibia should be sent for frozen section analysis to verify that the remaining bone is free of tumor. To form a nice conical stump, we recommend excising the fibula about 4 to 5 cm above the tibial osteotomy, in addition to removing some of the peroneal musculature at the same level. This permits easier stump shrinking and prosthetic fit (TECH FIG 1F).


Placement of Epineural Catheter and Myodesis
A small opening is made using a no. 15 blade scalpel into the epineural sheath. The epineural catheter, which has previously been flushed with 0.25% bupivacaine, is introduced into the epineural space and advanced proximally for 5 to 7 cm. The neural sheath is then closed with 4-0 chromic suture. A 16-gauge angiocatheter is introduced into the skin at the desired site of exit for the epineural catheter. The epineural catheter is then threaded through the angiocatheter until it is visible beyond the skin. The angiocatheter, encasing the epineural catheter, is carefully brought through the subcutaneous tissue to exit at the skin. Using drill holes in the distal tibia, the major muscle groups are attached to the bone with heavy sutures. The remaining muscle layers are used to make a circumferential covering layer over the bony stump (TECH FIG 2).

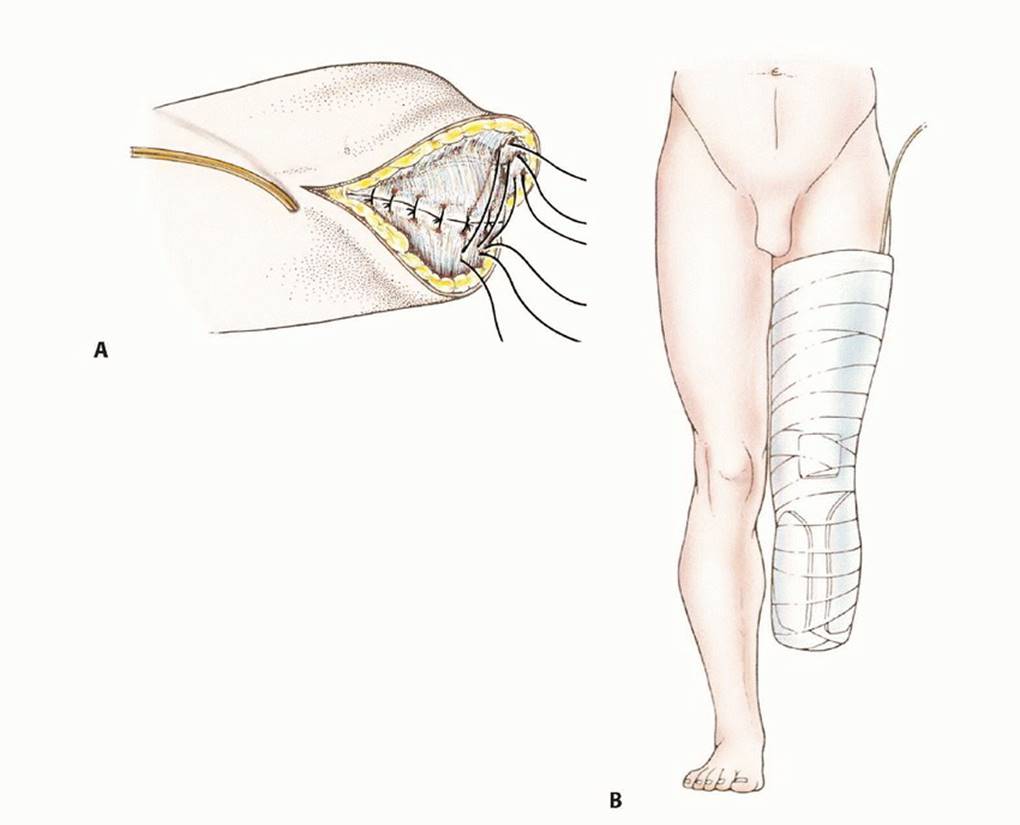
Drains and Skin Closure
Closed suction drains placed beneath the fascial layer are brought out of the medial and lateral aspects of the incision (TECH FIG 3A). The superficial fascia is tightly closed to prevent postoperative wound complications, which could delay prosthetic fitting. The surgeon should avoid having excess tissue and large skin folds during the skin closure, which could interfere with optimal prosthetic fitting. A rigid dressing is applied at the completion of the procedure with the knee in extension to prevent excessive swelling and development of a flexion contracture. After the initial rigid dressing is removed (usually 10 to 14 days following surgery), a stumpshrinker sock can be worn to decrease any remaining swelling (TECH FIG 3B).


PEARLS AND PITFALLS
- Stump contour - Rounding the contour of the distal end of the tibial stump and resecting the fibula a few centimeters shorter than the tibia can promote better fit and ease with prosthesis use.
- Myodesis - Functional myodesis of the major muscle groups of the leg to the distal tibia provides good soft tissue coverage for the stump while allowing functional range of motion.
- Wound healing problems - Healing can be compromised by preoperative chemotherapy. The use of drains and attention to detail with wound closures can help avoid these problems as well as hematoma and seroma development, which can delay other adjunctive treatments.
- Postoperative flexion contracture - The use of a knee immobilizer or custom splint can prevent the development of a flexion contracture.
- Phantom pain and causalgia - Perineural catheter flow rate and dose should be titrated, typically 4-8 mL of 0.25% bupivacaine per hour for about 72 hours.
POSTOPERATIVE CARE
Once the initial postoperative dressing is removed, a stumpshrinker sock can be worn to minimize swelling. Patients should be counseled that the transition to prosthesis use will be slow and gradual and will occur over about 3 to 6 months. Once an initial prosthesis can be fitted, wear time is gradually increased to build tolerance (FIG 4).

OUTCOMES
Similar to other lower extremity amputations, BKAs have been shown to be effective in palliation and improving the quality of life in cancer patients. As might be expected, patients after BKAs report less limitations than their AKA counterparts and are less likely to ambulate with walking aids or a
APA References
- Bahk WJ, et al. (2012). Effects of pneumatic tourniquet use on the outcomes of knee arthroscopy. Knee Surg Relat Res, 24(3): 153-9.
- National Academies of Sciences, Engineering, and Medicine. (2018). Below-Knee Amputation . National Academies Press.
- Al-Hassi HO, et al. (2021). Below-Knee Amputation Hutaif Orthopedic Hospital Journal, 7(1): 21-26.
- Yamaguchi A, et al. (2014). Below-Knee Amputation Oncology Letters, 8(5): 2089-2094.

