Open Reduction and Internal Fixation of the Sacroiliac Joint and Sacrum
DEFINITION
■Pelvic fractures are serious injuries associated with a diverse assortment of morbidities and mortality rates ranging from 0% to 50%.
■Fractures and dislocations of the pelvis involve, in broad terms, injuries to the anterior and posterior structures of the pelvic ring.
■Injuries to the anterior pelvic ring include symphyseal dis- ruption and pubic body or rami fractures.
■Injuries to the posterior pelvic ring involve iliac wing fractures, sacroiliac (SI) joint dislocations and fracture- dislocations, and sacral fractures.
■The implications and treatment of damage to these struc- tures vary widely with the broad spectrum of injury patterns, combinations of injuries, and degree of displacement.
■This chapter will focus on treatment of displaced sacral frac- tures and type 3 SI joint dislocations.
ANATOMY
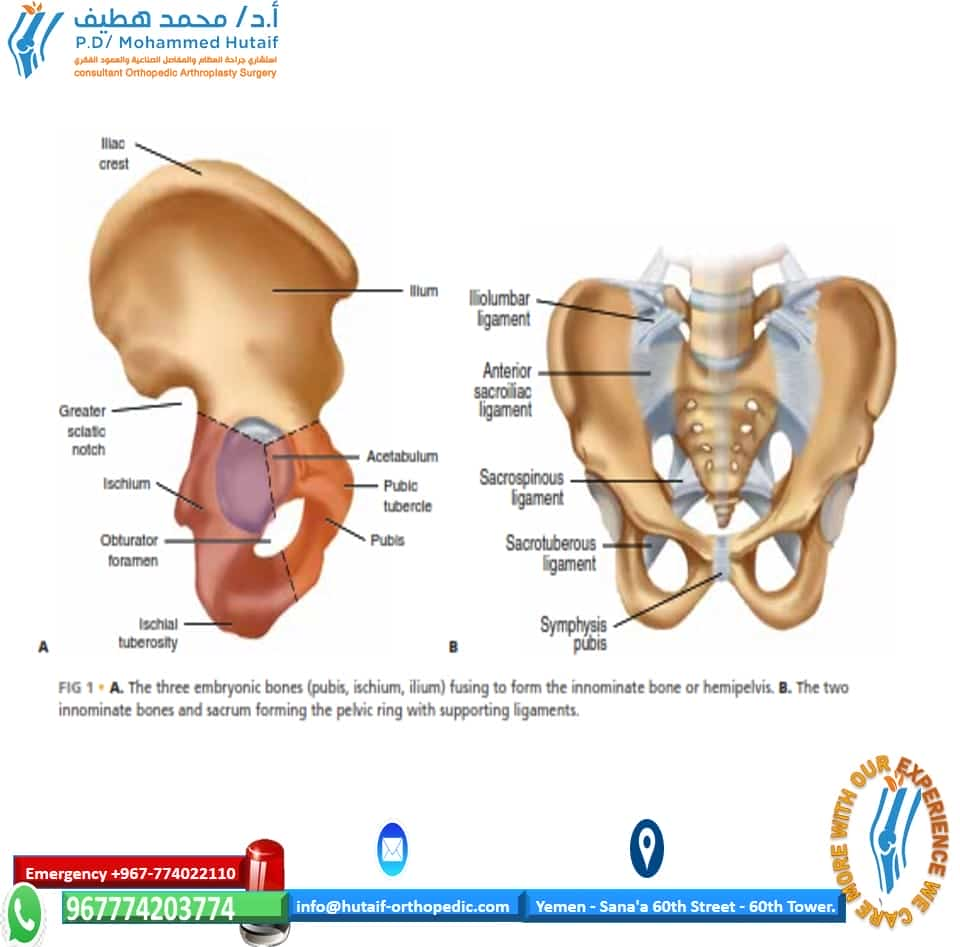
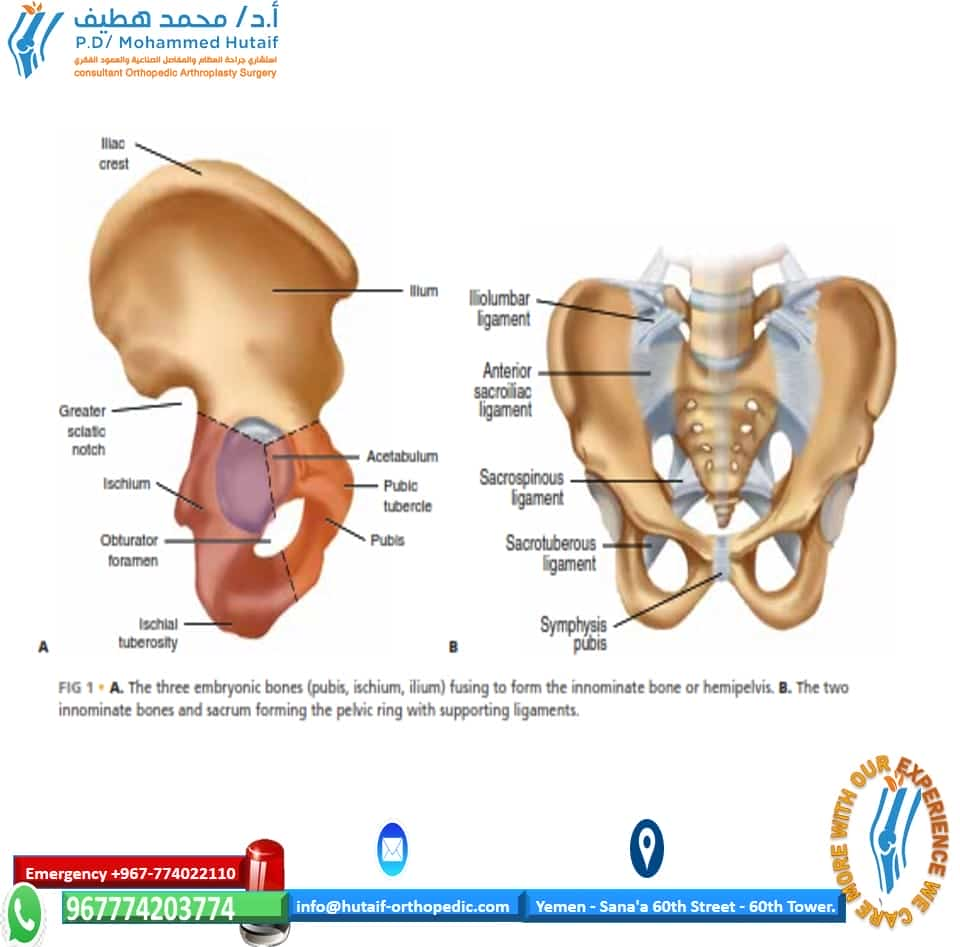
■The pelvis is a ring structure composed of the two hemipelves, or innominate bones, and the sacrum. Each innominate bone is formed as the result of fusion of the three embryonic bony ele- ments: the ilium, the pubis, and the ischium (FIG 1A).
■The two innominate bones are joined anteriorly at the pubic symphysis, a symphyseal joint. Posteriorly, the two innominate bones articulate with the wings, or alae, of the sacrum via the strong SI joints to complete the ring (FIG 1B).
■The sacrum represents the terminal structural segment of the spinal column that connects the pelvis and extremities to the trunk and spine.
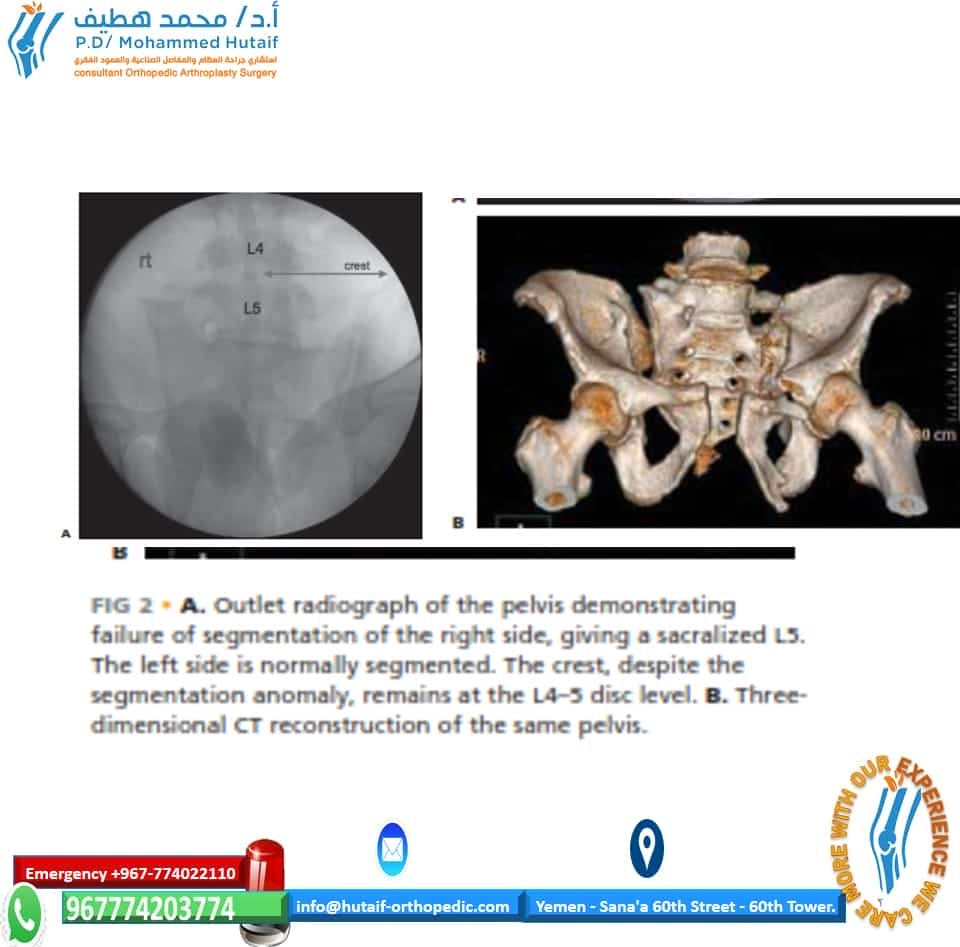
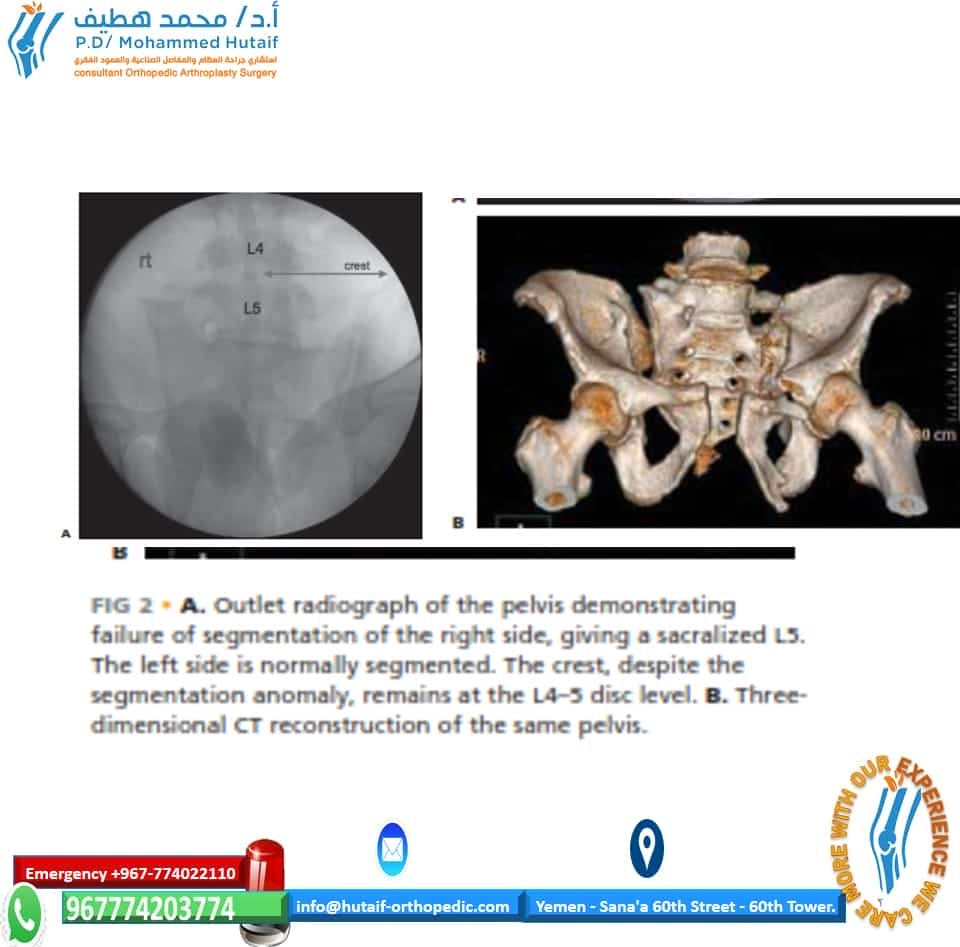
■As the sacrum is essentially a spinal element, it is subject to segmentation abnormalities and dysmorphisms.
■Most commonly, segmentation anomalies such as a lum- barized S1 and a sacralized L5 will be present (FIG 2).
■The only true way to be sure which defect, if any, is pres- ent, is to count down from the first thoracic vertebrae, which is the first vertebra to have transverse processes that are inclined cephalad.
■As a general rule of thumb, however, the top of the iliac crest is usually at the same level as the L4/5 disc space. This rule can be used to judge the presence of dysmorphism (see Fig 2A).
■These issues are pertinent to interpretation of the radi- ographic landmarks required to safely place iliosacral screws (see later).
■Being wedge-shaped, the sacrum forms a keystone articula- tion with the innominate bones.
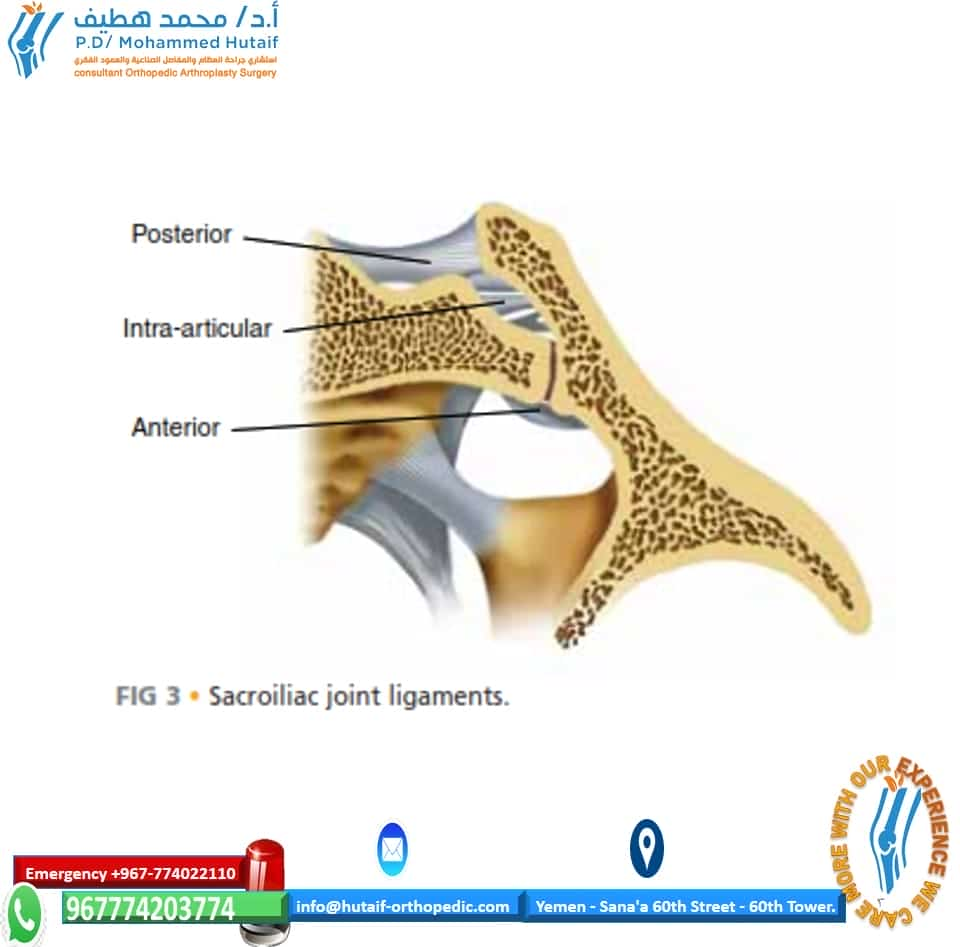
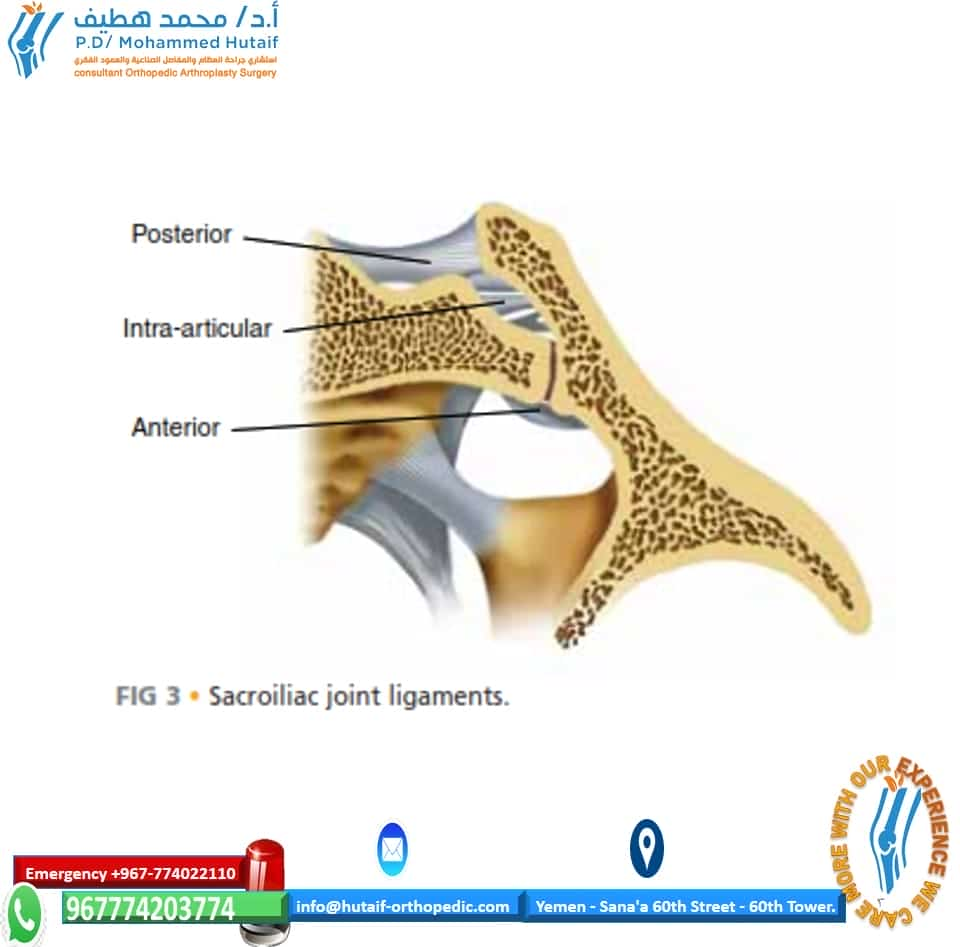
■By virtue of this shape and their orientation, the SI joints are inherently unstable and the maintenance of posterior pelvic ring integrity is wholly dependent on the support pro- vided by the ligamentous structures for stability (see Fig 1B and FIG 3).
■With axial loading, the natural tendency is for each hemipelvis to externally rotate and translate in a cephalad and posterior di- rection. The pelvic ligaments are structured and positioned to re- Iliac crest Ilium Iliolumbar ligament Greater sciatic notch Ischium Obturator foramen Acetabulum Pubic tubercle Pubis Anterior sacroiliac ligament Sacrospinous ligament Sacrotuberous ligament Ischial A tuberosity Symphysis B pubis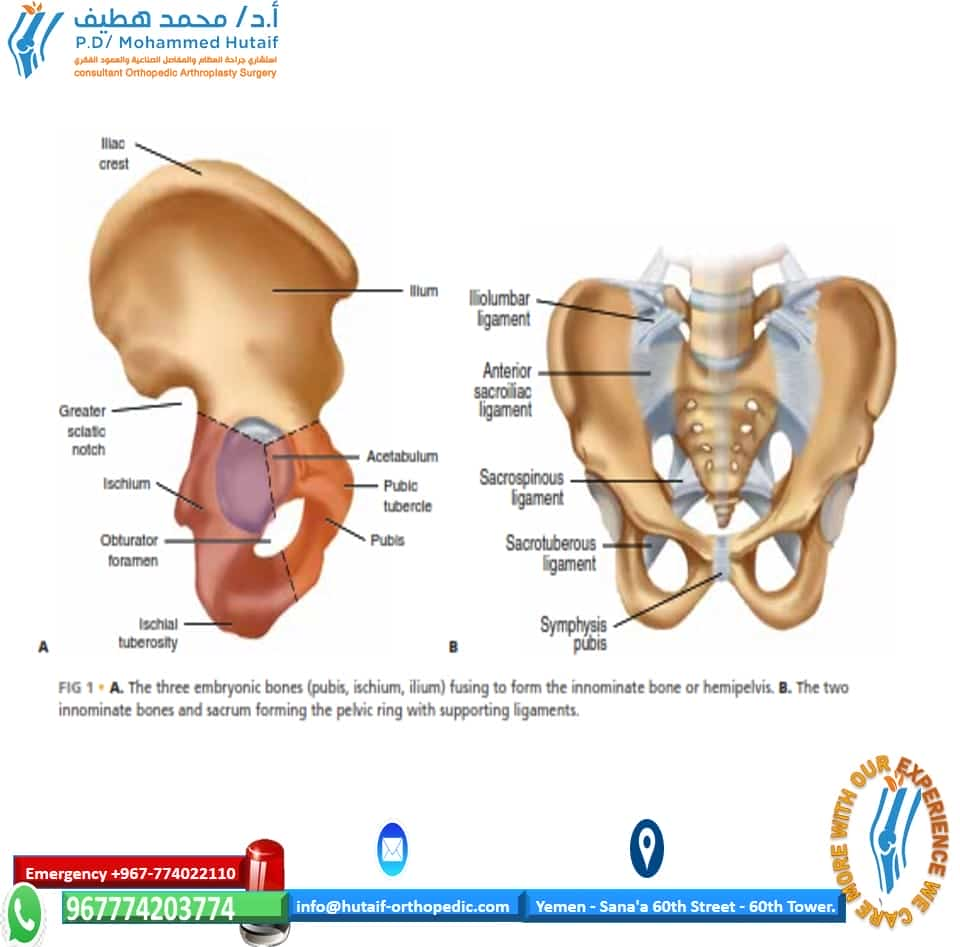
FIG 1 • A. The three embryonic bones (pubis, ischium, ilium) fusing to form the innominate bone or hemipelvis. B. The two innominate bones and sacrum forming the pelvic ring with supporting ligaments. 487 488
■The symphyseal ligaments (themselves contributing no more than 15% to pelvic ring stability), the sacrotuberous ligaments, and the sacrospinous ligaments resist external rotation.13,32
■The bladder is immediately posterior to the pubic bodies and symphysis, separated only by a thin layer of fat and the potential space of Retzius.
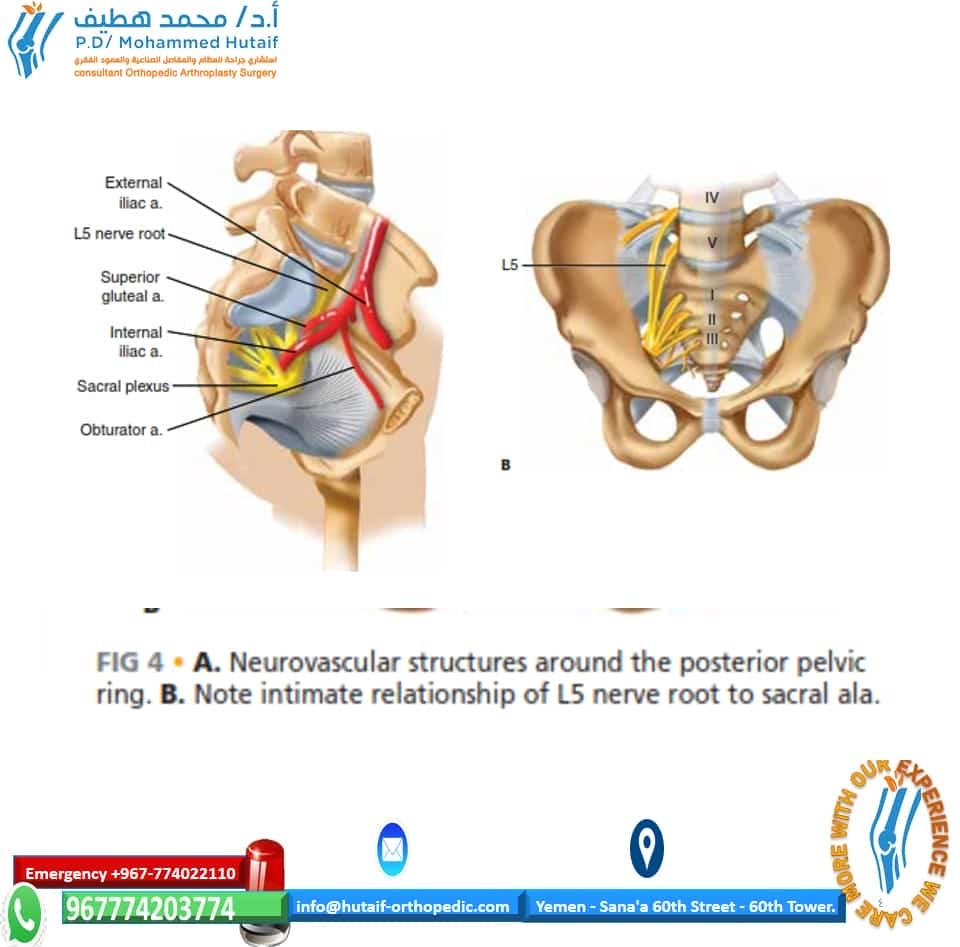
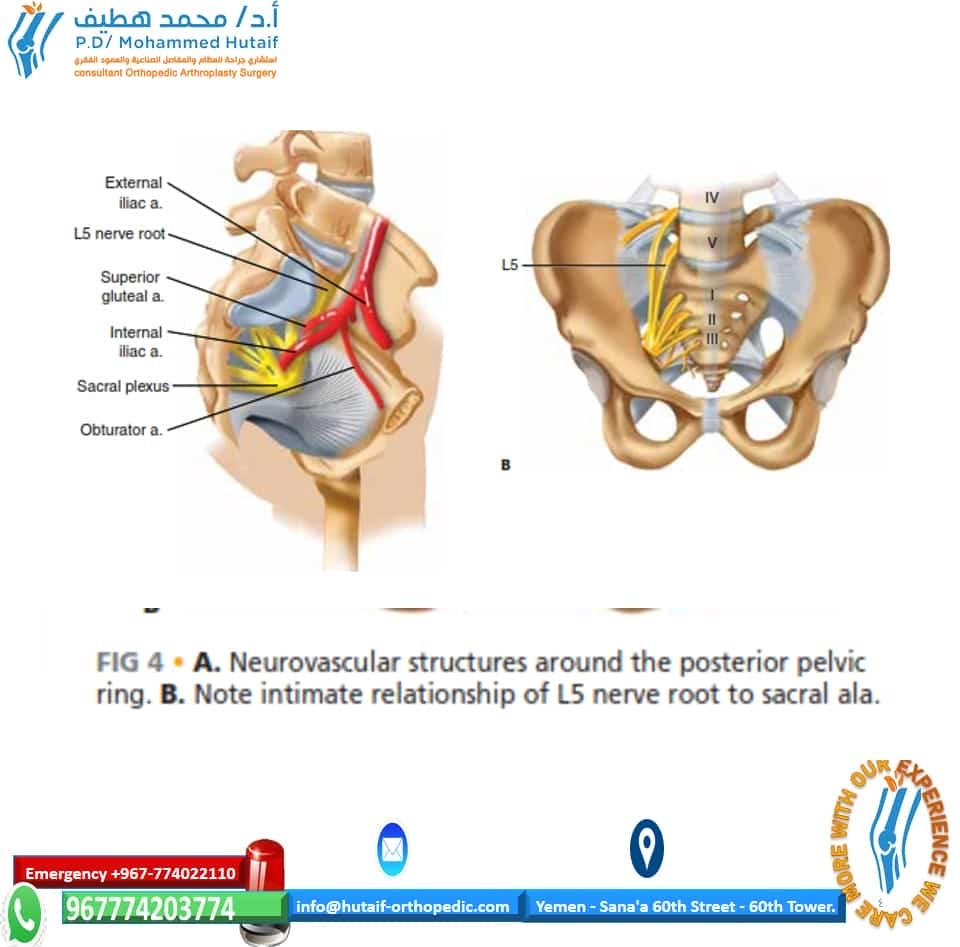
■The intimate relationship of the L5 nerve root to the supe- rior aspect of the sacral ala as it courses to join the lum- bosacral plexus is a key anatomic feature that must be kept in mind during reduction and stabilization of posterior pelvic ring injuries (FIG 4).
■The superior gluteal artery is immediately lateral to the in- ferior aspect of the SI joint as it arises from the internal iliac artery to exit the greater sciatic notch with the superior gluteal nerve. The obturator nerve and artery course along the quadrilateral plate (medial wall) of the acetabulum as they exit the superior and lateral quadrant of the obturator foramen (see Fig 4). A External iliac a. L5 nerve root Superior gluteal a.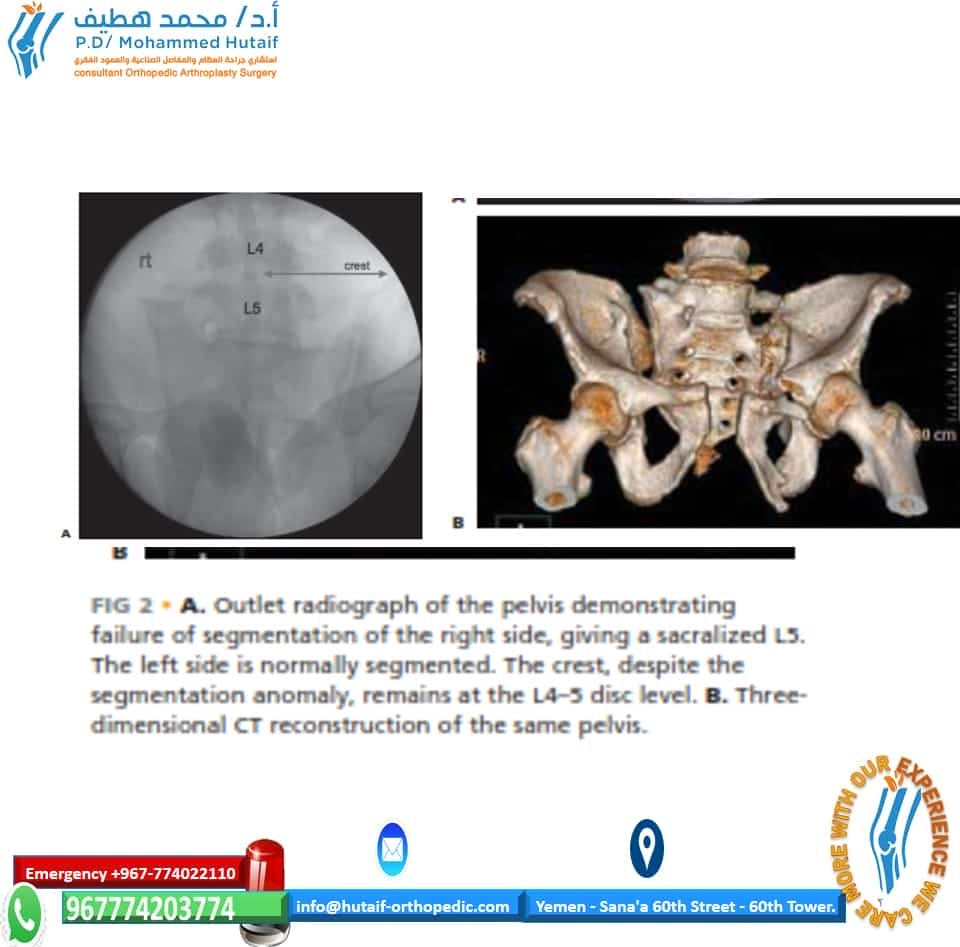
B FIG 2 • A. Outlet radiograph of the pelvis demonstrating failure of segmentation of the right side, giving a sacralized L5. The left side is normally segmented. The crest, despite the segmentation anomaly, remains at the L4–5 disc level. B. Three- dimensional CT reconstruction of the same pelvis. sist these deformations as static stabilizers of the pelvis. There are no specific dynamic stabilizers of the pelvic ring.
■The SI ligaments (anterior, posterior and intra-articular ligaments) are the strongest ligaments in the body, with the posterior SI ligaments being the most important in resisting A posterior and cephalad displacement (see Fig 3). Posterior L5 Intra-articular Anterior Internal iliac a. Sacral plexus Obturator a. B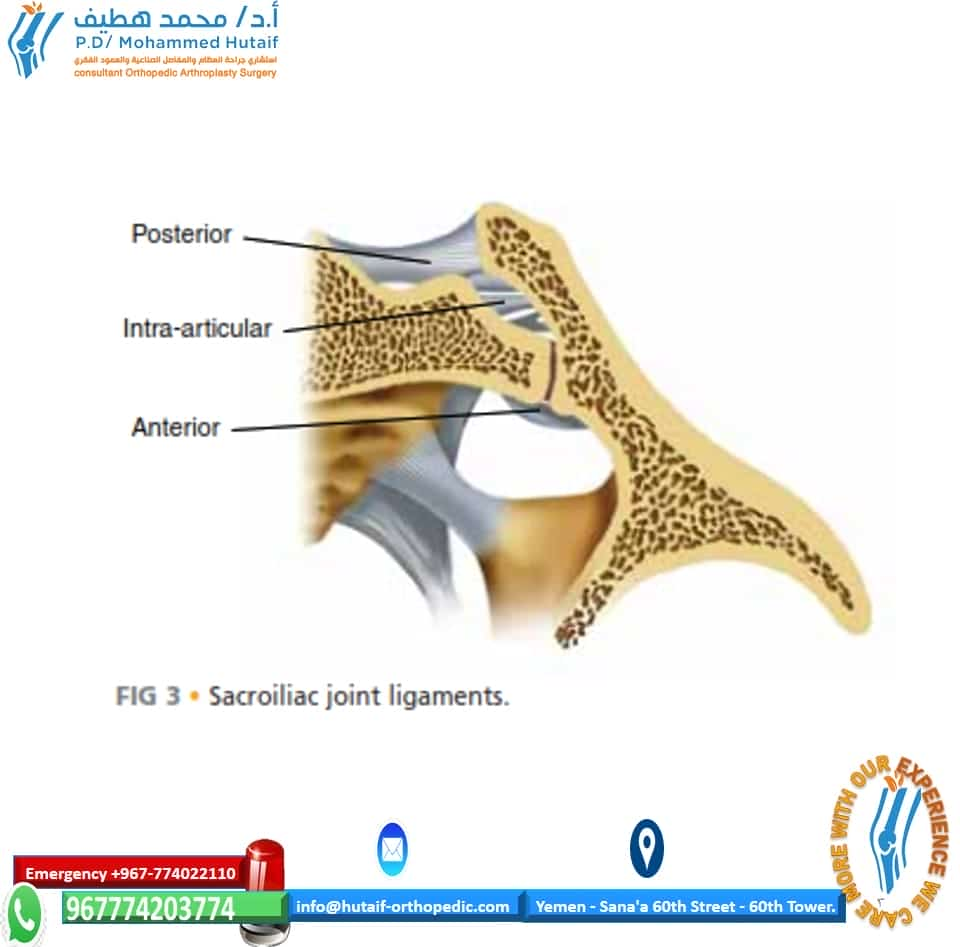
FIG 3 • Sacroiliac joint ligaments.
FIG 4 • A. Neurovascular structures around the posterior pelvic ring. B. Note intimate relationship of L5 nerve root to sacral ala.
PATHOGENESIS
■Because the SI ligaments are the most resilient in the human body, SI dislocations occur purely as a result of high-energy traumatic injuries.
■Anteroposterior compression of the pelvic ring causing external rotation of the innominate (which may or may not be coupled with a vertical shearing force) is the most com- mon cause of SI joint dislocation.
■Sacral fractures, however, can occur in three distinctly dif- ferent situations.
■Insufficiency fractures of the sacrum arise secondary to failure through excessively osteoporotic or ostepenic bone.
■Stress fractures of the sacrum result from fatigue and cyclic failure of normal bone in high-level athletes or mili- tary recruits.
■Traumatic disruptions result from high-energy lateral or anteroposterior compression or vertical shear injuries such as (in order of decreasing frequency) motorcycle crashes, auto–pedestrian collisions, falls from height, motor vehicle accidents, or crush injuries.13,32
NATURAL HISTORY
■Pelvic fractures occur in at least 20% of blunt trauma ad- missions, most frequently in young males.
■They can result in small insignificant fractures of the pubic rami with no compromise of pelvic ring stability, or major injuries and disruptions that can be associated with life-threatening bleeding or visceral injury.
■The pelvic ring encloses the true pelvis (organs contained below the pelvic brim, extraperitoneal) and the false pelvis (organs contained above the pelvic brim, both peritoneal and retroperitoneal).
■The most commonly associated injuries to structures con- tained within the true pelvis are the internal iliac arterial and venous systems and branches, the bladder (20%) and ure- thra (14%), the lumbosacral plexus, and the rectum and vaginal vault (open pelvic fractures).
■Injuries to structures within the false pelvis as a direct result of the pelvic fracture are uncommon, but severe iliac wing fractures with abdominal wall disruption can result in intesti- nal injury and even entrapment.
■Morbidity and mortality from pelvic fractures can be high and are most commonly secondary to pelvic hemorrhage.
■The mortality rate associated with pelvic fracture with an associated bladder rupture approaches 35% in some series, and the mortality rate of open pelvic fractures involving the perineum used to be as high as 50%.
■Fortunately, this has decreased to about 2% to 10% with the liberal use of diverting colostomies and more advanced stabilization techniques.
■Neurologic injury to the lumbosacral plexus can lead to sig- nificant sensorimotor dysfunction involving the extremities, bowel, bladder, and sexual functions.
■Because of these associated neurovascular and visceral in- juries, pelvic fractures often result in prolonged recovery peri- ods, significant chronic pain, permanent disability, and loss of psychological and socioeconomic structure.5,7,9,21–29
PATIENT HISTORY AND PHYSICAL FINDINGS
■Any patient presenting with a history of trauma or satisfy- ing criteria for a Trauma Alert in the emergency department should be suspected of having a pelvic fracture until otherwise ruled out by radiologic and physical examination.
■The physical examination should follow the primary and sec- ondary survey of the Advanced Trauma Life Support protocol.1
■Examination of a patient suspected of having a pelvic frac- ture should be divided into the examination of the abdomen, pelvic ring, perineum, rectum, vagina, and lower extremities.
■The abdominal examination should elucidate:
■Tenderness, fullness, or rigidity
■Abdominal wall disruptions, defects, or open wounds
■Flank ecchymosis
■Presence of internal degloving or a Morel-Lavalle lesion (separation of the subcutaneous tissues from the underlying fascia). This can be recognized by subcutaneous fluctuance or a fluid wave and, later, extensive ecchymosis.
■The rectal and vaginal examination should consider:
■The position of the prostate (a high-riding prostate may be a sign of urethral injury)
■Palpable bony fragments perforating the rectal or vaginal mucosa
■Defects or tears in the wall of the rectum or vagina indi- cating possible bony penetration
■Rectal or vaginal bleeding indicating possible tears or bony penetration
■Urethral bleeding at the meatus indicating possible ure- thral or bladder disruption
■Scrotal or labial swelling and ecchymosis indicating pelvic hemorrhage (FIG 5)
■Rectal tone, perianal sensation, voluntary sphincter con- trol, and bulbocavernosus reflex to assess for the presence of cauda equina syndrome or lower sacral nerve root injury
■Examination of the pelvic ring and extremities should focus on the following key factors:
■Palpable internal or external rotation instability of the pelvic ring with manually applied anteroposterior and lateral compressive forces on the iliac wings and crests
■Leg-length discrepancy with asymmetrical internal or ex- ternal rotation
■Neurologic status in patients able to comply can be assessed as follows:
■L1/2: iliopsoas (hip flexors) and upper anterior thigh sensation
■L3/4: quadriceps (knee extensors) and lower anterior thigh and medial calf sensation
■ L5: extensor hallucis longus, digitorum longus (toe dorsiflexion), peroneal eversion (although this can have a FIG 5 • Scrotal ecchymosis from internal pelvic hemorrhage. strong L4 component) and lateral calf and dorsum of foot sensation
■S1: gastrocsoleus complex (ankle plantarflexion) and pos- terior calf sensation
■S2/3: flexor hallucis and digitorum longus (toe plantar flexion) and sole of foot sensation
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain Radiographs
■The standard anteroposterior (AP pelvis) view should be part of the initial trauma series screening. With enough expe- rience, many of the injuries to the posterior pelvic ring can be diagnosed with this single projection (FIG 6A,B).
■A good AP radiograph should have the pubic symphysis co-linear with the sacral spinous processes.
■This allows side-to-side comparison of bony landmarks to aid in diagnosis of subtle displacements of the sacrum or SI joint.
■The cortical density of the pelvic brim and iliopectineal line should be traced back to its intersection with the lateral margin of the sacral ala.
■This intersection should be at the same level (usually the inferior margin of the S2 foramen) bilaterally.
■Asymmetry in the SI joint space and the appearance of the sacral foramina should alert the surgeon to the presence of an SI joint dislocation or sacral fracture.
■Fractures of the L5 transverse process may be a clue to a vertical shear injury that has avulsed the transverse process via the iliolumbar ligament.
■Symphyseal diastasis or displaced rami fractures should alert the examiner to additional injuries in the posterior ring, even though they may not be readily apparent on first glance.
■The inlet projection is taken with the x-ray beam directed caudally about 45 degrees to the radiographic film.
■A true inlet view of the pelvis, however, may require vari- ations on this degree of angulation because of the normal variations in sagittal plane pelvic obliquity.
■This view simulates a direct view into the pelvis from above along its longitudinal axis (FIG 6C,D).
■The inlet view is helpful in imaging:
■External or internal rotation of the hemipelvis
■Opening of the SI joint or an impaction fracture of the sacrum
■“AP” displacement or translation of the hemipelvis (see below)
■The outlet projection of the pelvis is obtained by directing the x-ray beam about 45 degrees cephalad to the radiographic film.
■This view simulates looking at the sacrum and SI joints di- rectly en face (FIG 6E,F).
■The outlet view is helpful in imaging:
■Cephalad or “vertical” shift of the hemipelvis
■Sacral fractures relative to the foramina
■Flexion–extension deformity of the hemipelvis
■These radiographs are taken at about 45 degrees to the long axis of the patient’s body.
■Therefore, a given amount of translation or displace- ment seen on the inlet or outlet view is in fact the sum of displacement vectors in both the coronal and axial planes. For example, “posterior” shift seen on the inlet projection is in fact a combination of both posterior and cephalad translation.
■Another important point to bear in mind is the appearance of the sacrum on the AP projection.
■If one sees a paradoxical inlet view of the upper sacrum and outlet view of the distal sacrum, a lateral radiograph and CT scan with sagittal reconstruction must be performed to rule out an occult sacral fracture-dislocation (a U-shaped
F FIG 6 • A,B. AP pelvis radiographs. Ideal film should have symphysis aligned with sacral spinous processes. C,D. Inlet pelvic radiographs. Note sacral promontory and alar regions. E,F. Outlet pelvic radiographs. Note sacral foramina and sacroiliac joints. Ideal image should have top of symphysis–rami at the S2–3 level.
B FIG 8 • A. Axial CT scan of transforaminal (Denis zone 2) sacral fracture. B. Axial CT scan of sacroiliac joint dislocation. Note di- astasis of anterior and posterior joint. C FIG 7 • A. AP radiograph of patient with a U-shaped sacral fracture. Note inlet view of proximal sacrum but outlet appear- ance of caudal sacrum. Axial (B) and sagittal (C) CT scan recon- structions of the same patient with a U-shaped sacral fracture. The fracture almost always occurs at the level of the vestigial disc space at S1–2. sacral fracture otherwise known as spinal-pelvic dissociation; FIG 7).
Computed Tomography
■CT is imperative in any suspected pelvic ring injury.
■As the pelvis is a ring structure, any disruption in one loca- tion (no matter how seemingly insignificant) must (by virtue of ring structure mechanics) be accompanied by disruption in another location.
■Three-millimeter axial sections (or 3 mm of vertical travel per 360-degree rotation of the gantry in a spiral CT) are rec- ommended to disclose the majority of significant injuries and to allow for good-quality three-dimensional reconstructions (FIG 8). Retrograde Urethrography and Cystography
■Retrograde urethrography and cystography are mandatory in pelvic fractures with ring disruption to rule out urethral and bladder injury.
■The Foley catheter is partially inserted into the urethra, and the balloon is inflated with 2 to 3 mL of sterile saline to oc- clude the urethra. Ten to 15 mL of water-soluble contrast is then injected into the urethra and the outlet view of the pelvis is repeated.
■If no extravasation is seen, the catheter is advanced into the bladder with injection of a further 300 mL of water-soluble contrast to rule out a bladder rupture. If no contrast extrava- sation is noted, the bladder is drained with the Foley, and any residual dye is noted.
■If passage of the catheter is not possible or there is a tear of the urethra or bladder neck, suprapubic catheterization should be performed well above the umbilicus if possible (to avoid contamination of potential future anterior pelvic operations). Pelvic Angiography
■Angiography is indicated in patients with persistent hemo- dynamic instability despite10:
■Adequate volume resuscitation
■Other sources of hemorrhage being ruled out (abdomen, thorax, and long bone fractures)
■Attempts to “close” the pelvic ring (see below) have failed to stop pelvic hemorrhage
■Most cases of pelvic hemorrhage (85%) arise from venous bleeding, which is not amenable to angiographic embolization.
■Arterial bleeding is usually from branches of the internal iliac system (median sacral, superior gluteal, pudendal, or obturator arteries; FIG 9).
FIG 10 • TPOD pelvic binder. (Courtesy of MidMed, Queensland, Australia.) B FIG 9 • Angiograms showing extravasation and embolization of superior gluteal artery. (Courtesy of Prof. Johannes Reuger.)
■If diagnostic peritoneal lavage is being performed to rule out abdominal hemorrhage, then it must be performed above the umbilicus and arcuate line to avoid false-positive results from pelvic hemorrhage.
NONOPERATIVE MANAGEMENT
■As a general rule, traumatic type 3 SI dislocations should not be managed nonoperatively.
■Progressive cephalad displacement of the hemipelvis will result in pelvic malunion. Leg-length inequality, chronic me- chanical low back and buttock pain, pelvic obliquity with sitting imbalance, and dyspareunia are common complaints when the hemipelvis and ischial tuberosities are positioned medially or cephalad.
■For patients in extremis or those with sepsis or critical med- ical comorbidity, nonoperative therapy may be the only option.
■In these cases, the pattern of deformity dictates the ma- neuvers to be used to minimize the malunion.
■Patients with any evidence of vertical instability should be placed into balanced longitudinal skeletal traction in an at- tempt to reduce or prevent further cephalad displacement.
■Distal femoral traction is preferable.
■Patients with external rotation deformity of the pelvic ring (ie, “open book” pelvis) should be initially treated with some form of temporizing pelvic binder (ie, the T-POD pelvic binder, Bio-Cybernetics, LaVerne, CA) or an external fixa- tion clamp.
■This helps to reduce the external rotation deformity, sta- bilize the pelvic hemorrhage and clot, and improve patient comfort in the acute resuscitative period.2
■Ideally, circumferential devices such as pelvic binders (FIG 10) should be applied over the greater trochanters, and frequent skin checks are mandatory to prevent full-thickness pressure ulceration. As such, they are rarely if ever indicated for definitive treatment. Anterior pelvic external fixators can be applied either in the iliac crest or the anterior inferior iliac spine and supra-acetabular bone.
■Anterior external fixators are good for controlling exter- nal and internal rotation of the anterior pelvic ring. Thus, the surgeon may elect to use them definitively if the SI joint is disrupted only through the anterior SI ligaments (a type 2 injury with no vertical or sagittal plane instability) or with certain lateral compression injuries where the sacral fracture is stable by virtue of its impaction.
■By themselves, however, anterior external fixators are not effective in controlling the posterior pelvic ring, and if applied incorrectly they can make some pelvic deformities worse.16,30
■For external fixation control of the posterior ring, external C-clamps and pelvic clamps are used on occasion, but expertise is required in their use to prevent serious complications from misplacement.8,18
■In contrast to SI joint dislocations, most traumatic sacral fractures can be treated successfully with nonoperative care.
■Although vertical shear sacral fractures represent the far end of the spectrum of unstable sacral fractures needing operative stabilization, impacted sacral fractures resulting from lateral compression mechanisms can be relatively sta- ble injuries (FIG 11A,B).
■If the radiographic and CT scanning evaluation reveals an impacted sacral alar fracture without significant displacement in other planes, a trial of nonoperative therapy is warranted. The patient must comply with the weight-bearing restrictions and close radiographic follow-up to prevent gradual shift that will result in a pelvic malunion and leg-length inequality with sitting imbalance (FIG 11C).
■Often, the presentation of the patient in bed can help to pre- dict success with nonoperative treatment of impacted sacral fractures.
■Patients able to roll in bed on their own and help with hy- gienic care with only minimal or moderate discomfort often have a relatively stable pelvis and will be able to mobilize with physical therapy.
■Some patients, however, will not be able to tolerate even log-rolling in the bed with nursing care.
■They may be found on examination under anesthesia to have an unstable pelvis despite innocuous-appearing imag- ing studies.
FIG 11 • A,B. Impacted sacral fracture from lateral compression mechanism with internal rotation. C. Nonoperative treatment of vertical shear sacral fracture with resultant malunion and leg-length inequality.
■If a patient with an impacted sacral fracture is deemed to be a candidate for nonoperative treatment, he or she is mobilized with physical therapy in 3 to 5 days so long as all other injuries permit.
■The patient is instructed in touch-down weight bearing on the affected extremity.
■If the patient can successfully mobilize, then AP, inlet, and outlet radiographs are repeated within a week to assess for any further displacement and increasing leg-length inequality.
■If no further displacement occurs, the patient is instructed to continue touch-down weight bearing for another 8 to 10 weeks, with repeat radiographs every 4 weeks.
NEXT