"Unlocking the Secrets of Kienbock Disease: Diagnosis and Prognosis Revealed"
Welcome to a scientific overview of Kienbock's Disease, a rare condition that causes avascular necrosis of the lunate bone in the wrist. In this article, we will explore the scientific aspects of the disease, including its epidemiology, etiology, anatomy, classification, presentation, imaging techniques, treatment options, and prognosis. Additionally, we will introduce tables to present relevant data more efficiently. So let's dive in!
Epidemiology
Kienbock's Disease most commonly affects males between the ages of 20 and 40. It is associated with various risk factors such as a history of trauma.
Etiology
The pathophysiology of Kienbock's Disease is thought to result from multiple factors, including biomechanical and anatomical factors. Biomechanical factors such as ulnar negative variance and repetitive trauma can lead to increased radial-lunate contact stress. Anatomical factors, including the geometry of the lunate and vascular supply, also play a role in the development of the disease.
Anatomy
The blood supply to the lunate bone can vary with three main patterns: Y-pattern, X-pattern, and I-pattern. Understanding these variations is essential for diagnosing and treating Kienbock's Disease.
| Lunate Blood Supply Patterns | Incidence |
|---|---|
| Y-pattern | ? |
| X-pattern | ? |
| I-pattern | ? |
Classification
Lichtman Classification
| Stage | Description | Treatment |
|---|---|---|
| Stage I | 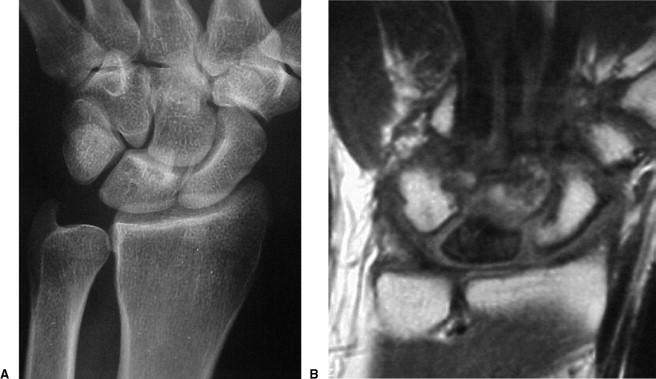 |
No visible changes on x-ray, changes seen on MRI Immobilization and NSAIDS |
| Stage II |  |
Sclerosis of lunate Joint leveling procedure (ulnar negative patients) Radial wedge osteotomy or STT fusion (ulnar neutral patients) Distal radius core decompression Revascularization procedures |
| Stage IIIA | 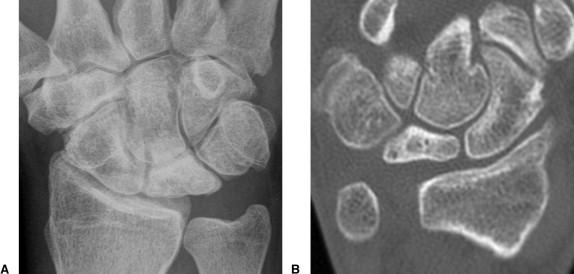 |
Lunate collapse, no scaphoid rotation Same as Stage II above |
| Stage IIIB |  |
Lunate collapse, fixed scaphoid rotation Proximal row carpectomy, STT fusion, or SC fusion |
| Stage IV | 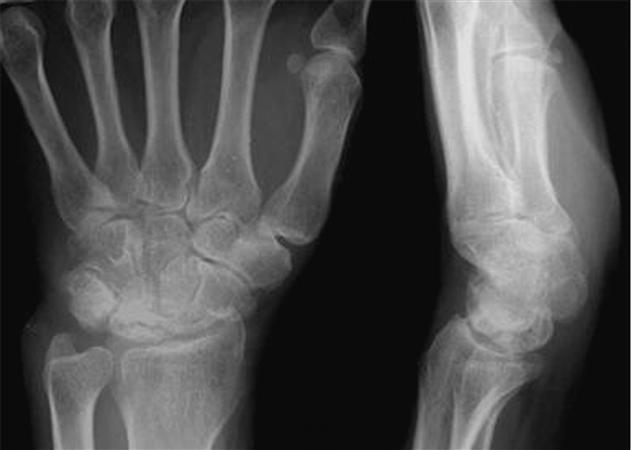 |
Degenerated adjacent intercarpal joints Wrist fusion, proximal row carpectomy, or limited intercarpal fusion |
Presentation and Diagnosis
Kienbock's Disease is usually characterized by dorsal wrist pain, particularly during activities. Physical examination often reveals tenderness and swelling around the radiocarpal joint. To diagnose the disease, various imaging techniques, such as radiographs, MRI, and CT scans, are used.
Imaging Findings
| Imaging Technique | Findings |
|---|---|
| Radiographs | Changes in bone shape, extent of disease |
| MRI | Early disease detection, reduced vascularity |
| CT | Detailed bone damage assessment |
Treatment Options
The treatment of Kienbock's Disease depends on the stage and severity of the disease. Nonoperative management, such as observation, immobilization, and NSAIDs, is appropriate for minimally symptomatic patients in the early stages. However, more severe cases and symptomatic patients may require surgical intervention.
A variety of operative procedures are available based on the severity of the disease and patient's symptoms. These include:
- Temporary scaphotrapeziotrapezoidal pinning
- Joint leveling procedures
- Radial or ulnar osteotomies
- Revascularization procedures
- Distal radius core decompression
- Partial wrist fusions
- Proximal row carpectomy (PRC)
- Wrist fusion
- Total wrist arthroplasty
| Operative Procedure | % Decrease on Radiolunate Contact Stress |
|---|---|
| Scaphotrapeziotrapezoidal fusion | 3% |
| Scaphocapitate fusion | 12% |
| Capitohamate fusion | 0% |
| Ulnar lengthening of 4mm | 45% |
| Radial shortening of 4mm | 45% |
| Capitate shortening and capitohamate fusion | 66%, with 26% increase in radioscaphoid load |
Prognosis
The prognosis for Kienbock's Disease varies depending on the stage of the disease and the chosen treatment approach. Early detection and diagnosis are essential for better outcomes. With proper care, patients can recover and regain normal wrist function.
In conclusion, Kienbock's Disease is an intriguing condition that affects the wrist and can cause significant pain and debilitation. Early diagnosis and appropriate treatment can help patients manage symptoms and improve their quality of life. If you suspect Kienbock's Disease, consult a healthcare professional for a proper evaluation and treatment plan.
Key Points
- Kienbock's Disease is the avascular necrosis of the lunate, leading to wrist pain and abnormal carpal motion.
- Incidence is highest in males between 20-40 years old.
- Risk factors include a history of trauma.
- Ulnar negative variance and decreased radial inclination increase radial-lunate contact stress, leading to the disease.
- Repetitive trauma and anatomic factors such as lunate geometry and vascular supply also play a role in the development of Kienbock's Disease.
- Diagnosis can be made with wrist radiographs, but MRI may be needed for early disease detection.
- Minimally symptomatic patients may be treated with NSAIDs and observation.
- Operative procedures may be considered depending on the severity of the disease and patient's symptoms.
- Patients with adolescent radiographic evidence of Kienbock's and progressive wrist pain are candidates for temporary pinning.
- Stage I, II, and IIIA disease with ulnar negative variance may be treated with joint leveling procedures such as radial shortening osteotomy or ulnar lengthening.
- Stage I, II, IIIA disease with ulnar positive or neutral variance may require radial wedge osteotomy or STT fusion.
- Stage I, II, IIIA, and IIIB disease may be treated with vascularized bone grafts.
- STT fusion, scaphocapitate fusion, or proximal row carpectomy may be performed for Stage II and IIIA or IIIB disease.
- Wrist fusion or total wrist arthroplasty may be necessary for Stage IV disease.
- The use of vascularized bone grafts and temporary pinning techniques may help improve outcomes.
- If unrecognized and untreated, Kienbock's Disease can progress and become debilitating.
Kienbock's Disease is the avascular necrosis of the lunate, leading to wrist pain and abnormal carpal motion.
Incidence is highest in males between 20-40 years old. Risk factors include a history of trauma.
Ulnar negative variance and decreased radial inclination increase radial-lunate contact stress, leading to the disease. Diagnosis can be made with wrist radiographs, but MRI may be needed for early disease detection.
Minimally symptomatic patients may be treated with NSAIDs and observation. Operative procedures may be considered depending on the severity of the disease and patient's symptoms.

