Cases of Intra-Articular Phalangeal Fractures
A case study of a 12-year-old female with an intra-articular phalangeal fracture. Includes clinical photos, treatment strategy, and outcome.
Contents
- Clinical History
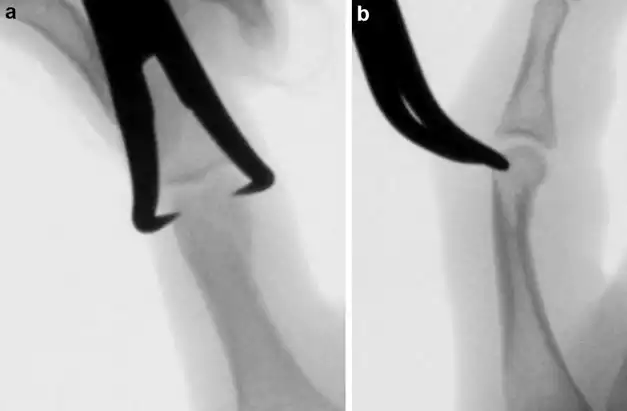
- Preoperative Clinical Photos and Radiographs
- Preoperative Problem List
- Treatment Strategy
- Basic Principles
- Images During Treatment
- Technical Pearls
- Outcome Clinical Photos and Radiographs
- Avoiding and Managing Problems
- Cross-References
- References and Suggested Reading
1 Clinical History
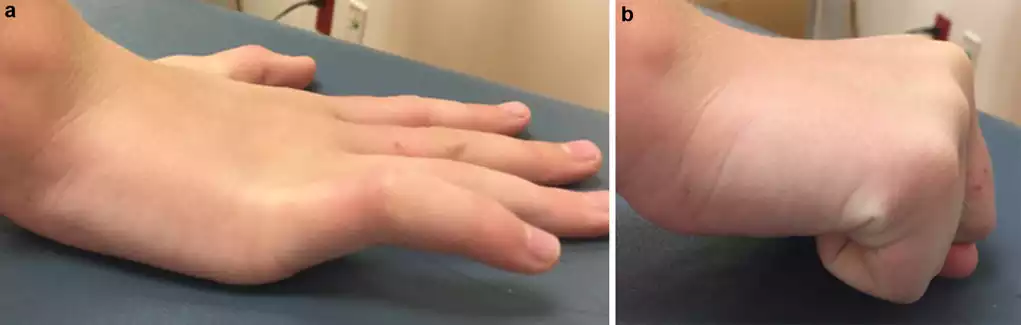
A 12-year-old female sustained an intra-articular fracture of the phalangeal head during basketball practice. She initially ignored the injury but eventually sought medical attention due to swelling, ecchymosis, limited range of motion, and tenderness at the fracture site. Malrotation of the digit was also observed due to fracture displacement. Given the intra-articular nature of the fracture, closed reduction and percutaneous pinning were necessary to restore joint congruity and stability while avoiding potential complications associated with open reduction.
2 Preoperative Clinical Photos and Radiographs


3 Preoperative Problem List
- Unstable, displaced articular fracture of the proximal interphalangeal joint
- Difficulty achieving reduction due to oblique fracture plane and delayed presentation
- Selection of fracture fixation method and postoperative immobilization
- Postoperative rehabilitation to restore full digit function
4 Treatment Strategy
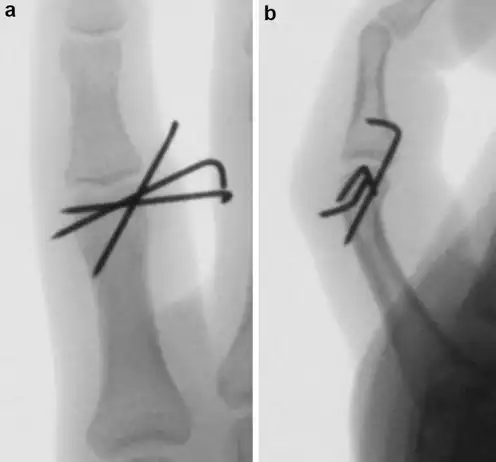
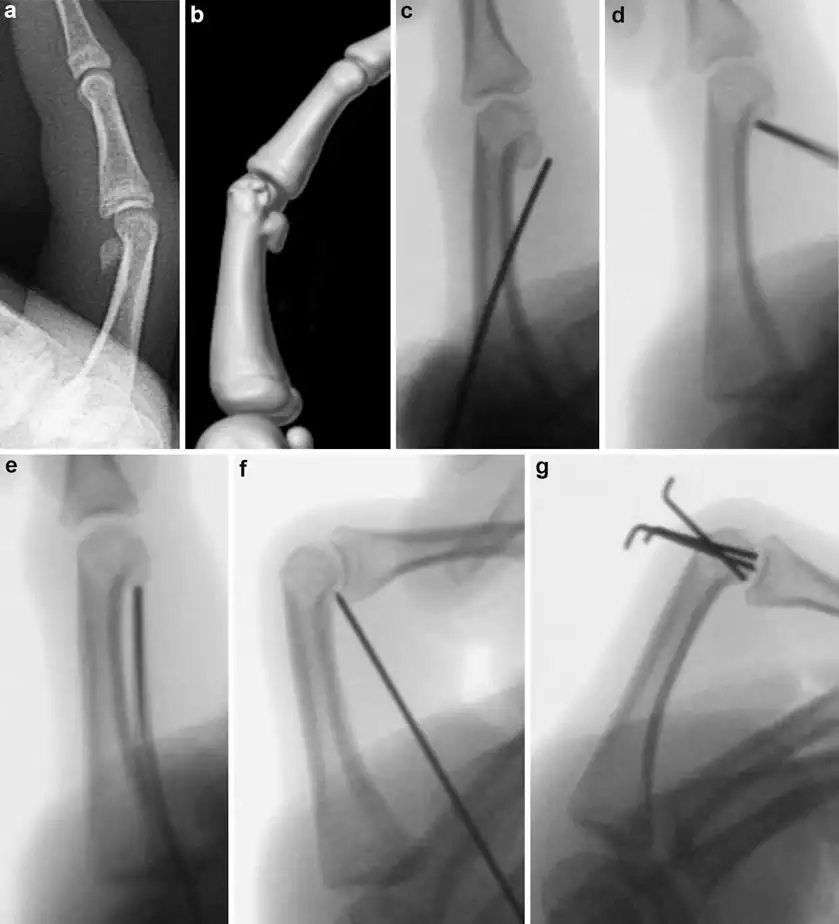
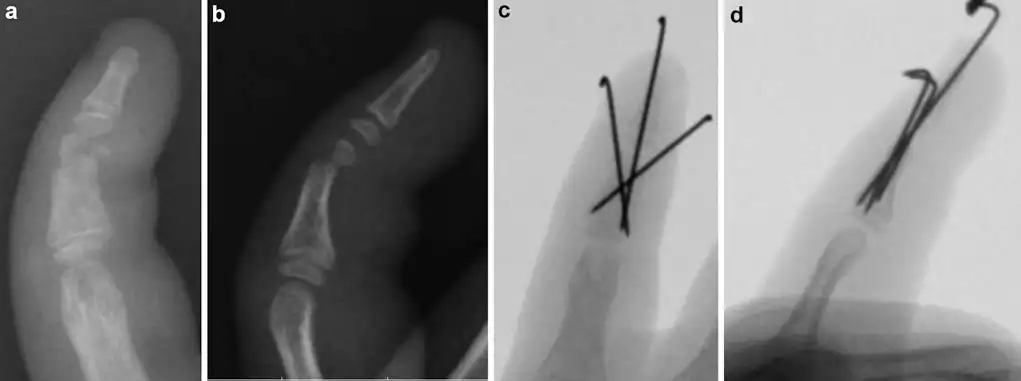
Due to the unstable nature of the fracture, static splinting or casting was not a suitable treatment option. The patient underwent closed reduction with the aid of a tenaculum clamp to restore articular congruity. Closed reduction with percutaneous pinning using Kirschner wires was then performed to stabilize the fracture. The pins were bent and cut outside the skin to facilitate easy removal. The patient was placed in an ulnar gutter cast and scheduled for pin removal after 4 weeks.
5 Basic Principles
The surgical goal is to achieve fracture reduction with congruent and level articular surfaces for proper healing. Closed reduction is typically performed using longitudinal traction and extension, with the assistance of a tenaculum clamp if necessary. Kirschner wires are used for stabilization, placed perpendicular to the fracture planes to provide optimal stability. After surgery, the wires are covered with a cast and kept in place for 4 weeks before removal.
6 Images During Treatment
7 Technical Pearls
- Close monitoring and examination of nondisplaced fractures is crucial, as they may become displaced over time if not stabilized surgically.
- Percutaneous reduction is preferred to limit soft tissue dissection and potential compromise of blood supply to the condyle.
- Different starting points and angles are used for Kirschner wires depending on the fracture type and location.
- Collateral ligament excursion should not be hindered by the Kirschner wires, as it may limit passive range of motion.
- Complex fractures may require multiple wires to adequately stabilize all fragments.
8 Outcome Clinical Photos and Radiographs


9 Avoiding and Managing Problems
- Ensure appropriate stabilization for nondisplaced fractures to prevent loss of reduction.
- Consider using multiple Kirschner wires or lag screws for unicondylar fractures to minimize the risk of displacement.
- Participate in postoperative occupational therapy to regain functional digit motion.
- Early active motion and stable fixation can help minimize joint stiffness.
- Limit soft tissue stripping to mitigate the risk of avascular necrosis.
- Address any long-term complaints, such as cold intolerance or chronic aching, through appropriate intervention.
10 Cross-References
References and Suggested Reading
- Bergeron L, Gagnon I, L'Ecuyer C, Caouette-Laberge L (2005) Treatment outcomes of unstable proximal phalangeal head fractures of the finger in children. Ann Plast Surg 54(1):28-32.
- Blazar P, Steinberg D (2000) Fractures of the proximal interphalangeal joint. J Am Acad Orthop Surg 8:383-390.
- Freeland A, Sud V (2001) Unicondylar and bicondylar proximal phalangeal fractures. J Am Soc Surg Hand 1(1):14-24.
- Weiss A, Hastings H (1993) Distal unicondylar fractures of the proximal phalanx. J Hand Surg 18(4):594-599.

