Retrograde Intramedullary Nailing of the Femur FRACTUREs
Retrograde Intramedullary Nailing of the Femur
DEFINITION
- Retrograde femoral nailing can be defined as any femoral nailing technique with a distal entry from the condyles or through an intercondylar, intra-articular starting point.
- For this chapter, retrograde femoral nailing will refer to nails with an intercondylar starting point that extend through the shaft region to the proximal femur. In certain fracture situations, shortened nails (supracondylar nails) can be used with the same starting point for fixation of distal femoral fractures.
ANATOMY
- The femoral shaft is tubular in shape over the extent of the isthmus, gradually flaring infraisthmally into the distal femur, which is trapezoidal in cross-section.
-
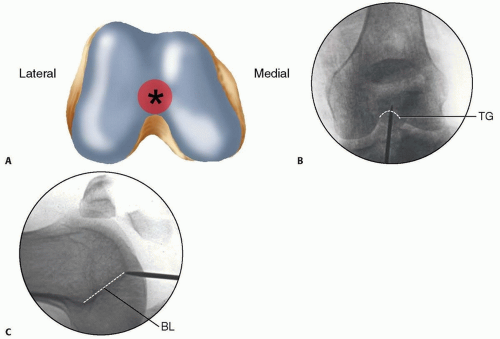
The entry point for the retrograde femoral nail is located at the distal end of the patellofemoral grove, just anterior to the posterior cruciate ligament insertion (FIG 1A).
- Radiographically, this is located in the midline or just medial to the midline between the condyles on the anteroposterior (AP) view and laterally just anterior to the line of Blumensaat as it meets the trochlear grove (FIG 1B,C).5, 12, 14, 15, 18 This flat articular area has minimal to no contact with the patella until 120 degrees of flexion.1, 5
|
FIG 1 • A. Distal femur viewed end on, with ideal starting point for retrograde femoral nailing identified (asterisk) just anterior to the posterior cruciate ligament insertion. B,C. AP and lateral radiographs of the knee, with the initial starting guidewire positioned at the ideal starting point for retrograde femoral nailing. The radiographic landmark for the trochlear groove (TG) is indicated on the AP radiograph and for the line of Blumensaat (BL) on the lateral radiograph.
FIG 1 • A. Distal femur viewed end on, with ideal starting point for retrograde femoral nailing identified (asterisk) just anterior to the posterior cruciate ligament insertion. B,C. AP and lateral radiographs of the knee, with the initial starting guidewire positioned at the ideal starting point for retrograde femoral nailing. The radiographic landmark for the trochlear groove (TG) is indicated on the AP radiograph and for the line of Blumensaat (BL) on the lateral radiograph. |
-
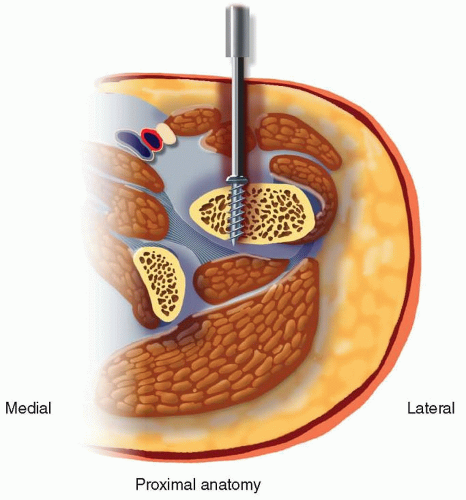
Pertinent proximal anatomy includes neurovascular structures anterior to the proximal femur, close to interlocking screw insertion sites.24
- The femoral artery is medial to the proximal femur, with branches that cross the anterior femur more than 4 cm distal to the lesser trochanter.
- Branches of the femoral nerve cross more proximal starting 4 cm distal to the piriformis fossa.
- Damage to neurovascular structures caused by proximal locking screw insertion can be avoided or minimized by avoiding medial dissection and with placement at or above the lesser trochanter (FIG 2).
PATHOGENESIS
- Femoral shaft fractures are markers of high-energy injuries.10, 12, 13, 14, 23, 27
-
Studies have shown that 38% of trauma patients diagnosed with a femoral shaft fracture have additional injuries.3, 7, 8, 26
- In femur fracture patients with associated injuries, the most common findings are other musculoskeletal injuries (93%), thoracic injuries (62%), head injuries (59%), abdominal injuries (35%), and facial injuries (16%).7
|
FIG 2 • Cross-sectional view of the proximal femur, with proximal interlocking screw insertion shown and pertinent medial neurovascular structures.
FIG 2 • Cross-sectional view of the proximal femur, with proximal interlocking screw insertion shown and pertinent medial neurovascular structures. |
- Ipsilateral femoral neck fractures occur in 1% to 6% of all femoral shaft fractures and are initially missed in up to 20% to 50% of cases.29 Recognition of these injuries before intramedullary stabilization is important to minimize potential complications (refer to section on Imaging and Other Diagnostic Studies).
- All trauma patients should undergo the standard advanced trauma life support (ATLS) examination to rule out associated life-threatening injuries.
- Although less common, femoral shaft fractures can occur in isolated sports injuries and in low-energy injuries associated with pathologic bone, such as with osteoporosis or metastatic bone disease.
PATIENT HISTORY AND PHYSICAL FINDINGS
- Pain and deformity of the thigh are usually obvious but may be obscured in the morbidly obese patient.
- The fractured limb should be closely examined to avoid missing any open wounds, particularly in the posterior aspect of the thigh. Skin abrasions and apparently minor wounds should be assessed to determine if they communicate with the fracture.
- Swelling is a common finding with femoral shaft fractures. Compartment syndrome of the thigh is rare but can occur.28
- The entire lower extremity and pelvis needs to be evaluated because of the high rate of associated musculoskeletal injuries.
- A thorough neurologic and vascular examination must also be performed. Although femoral nerve damage is very unusual, sciatic nerve damage can occur.4, 6, 34
- Associated ligamentous injuries of the knee are common but may be difficult to assess until definitive stabilization of the femur has been obtained. Therefore, this examination should be repeated after nailing the femoral fracture.31, 32
IMAGING AND OTHER DIAGNOSTIC STUDIES
-
AP and lateral radiographs of the full length of the femur are essential, as well as formal AP and lateral radiographs of the hip and knee.
- Lateral knee radiographs should be closely evaluated for subtle patellar impaction fractures or nondisplaced fractures.
- Hip radiographs should be closely examined to rule out an associated femoral neck fracture, which has been shown to occur in 1% to 6% of femoral shaft fractures.29
- Some surgeons recommend a routine computed tomography (CT) scan examination of the femoral neck as part of the trauma scan to rule out a femoral neck fracture.
- A reported 20% to 50% of these injuries are missed on the initial plain radiographic examination.29
- Any coronal fractures seen on CT examination should be considered a contraindication for retrograde nailing owing to the possibility of compromising the distal interlocking screw fixation.
- Because of the high association of missed coronal fractures in high-energy injuries, a CT scan of the knee should be obtained whenever formal knee radiographs reveal a supracondylar distal femur fracture and there is consideration for retrograde nailing.17
SURGICAL MANAGEMENT
Classifications and Relative Indications
-
It is important to assess the extent of the fracture both proximally and distally with proper radiographs.
- Proximally, CT scans can supplement plain radiographs to determine fracture line extension into the peritrochanteric region and to check for occult femoral neck fractures.
- Distally, CT imaging is helpful to assess intra-articular extension and to check for coronal plane fractures.17
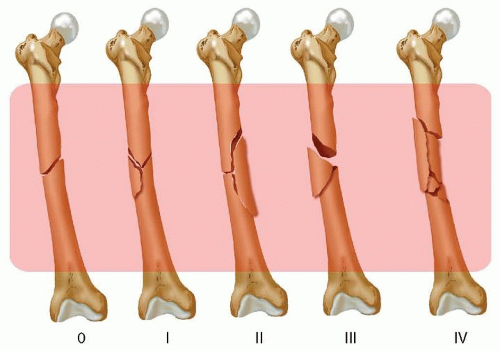
- All femoral shaft fractures, as classified by the Winquist system,33 are technically suitable for retrograde femoral nailing (FIG 3).
|
FIG 3 • Winquist femoral shaft fracture classification system.33 All fracture patterns in this system are amenable to retrograde femoral nailing
FIG 3 • Winquist femoral shaft fracture classification system.33 All fracture patterns in this system are amenable to retrograde femoral nailing. |
||||||||||||||||||||||||
|
Table 1 Relative Indications for Retrograde Intramedullary Nailing of the Femur |
||||||||||||||||||||||||
|
-
Retrograde femoral nailing is not considered to be the standard of care for treatment of more proximal subtrochanteric fractures, but in certain patient circumstances, it may be the treatment of choice (Table 1).
- Subtrochanteric fractures with the lesser trochanter and piriformis fossa intact, Russell-Taylor IA fractures (
- FIG 4),25 may be amenable to retrograde femoral nailing if other patient factors favor a retrograde approach.
- Ideally, some proximal medial cortex remains intact to act as a buttress against the nail.
- It is important to know how far the proximal interlocking screw holes are from the tip of the nail in the retrograde nail system available in your hospital.
- We recommend being able to obtain two bicortical interlocking screws above the most proximal fracture line for very proximal fractures. If possible, they should be through holes, not slots, in the nail to provide more stability.
- If the subtrochanteric fracture has proximal extension, including either the lesser trochanter or piriformis fossa, or both, then proximal interlocking screw fixation of the retrograde nail would be compromised and alternative fracture fixation methods should be considered.
- Retrograde femoral nailing may be considered in certain supracondylar distal femoral fractures. We find that Muller’s AO classification system of distal femoral fractures16 best elucidates which of these fractures can be addressed with retrograde femoral nailing (FIG 5).
- Consideration for retrograde femoral nailing can be given for all extra-articular (A subgroup) fractures.
- It is important to know the distance between the distal interlocking screw holes and the tip of the nail in the retrograde nail system available in your hospital.
- We recommend being able to obtain at least two bicortical interlocking screws below the most distal fracture line for distal fractures.
- Nails with oblique distal interlocking options can be advantageous because of increased stability and potentially less screw head prominence.