Information about ulnar styloid fractures and its treatment process
Learn how to perform arthroscopically assisted reduction of distal radius fractures and stabilize large ulnar styloid fragments with proper techniques.
Following anatomic reduction of the distal radius fracture, insert the arthroscope in the dorsal 3/4 portal and the probe in the 6R portal. Palpate the tension of the articular disc to check if the peripheral TFCC fibers are still attached to the proximal ulna. Repair arthroscopically if there is a peripheral tear of the articular disc. Stabilize a large ulnar styloid fragment when the articular disc is lax by palpation and no peripheral TFCC is identified using either a tension band technique or a micro headless cannulated screw.
Make a small incision between the extensor carpi ulnaris and the flexor carpi ulnaris tendons and identify the fracture site. Retrieve the distal fragment and mobilize the styloid fragment using a blade, taking care to protect the TFCC insertion. Reduce the fragment anatomically and stabilize it using either a tension band technique or a micro headless cannulated screw. Verify the fracture reduction with fluoroscopy and document restoration of TFCC tension with arthroscopy.
POSTOPERATIVE CARE
The degree of postoperative immobilization depends on numerous factors such as the mode of fracture stabilization, the quality of the bone for internal fixation, the stability of fixation, and the management of any associated soft tissue injuries that were addressed during the arthroscopic evaluation. Immediate range of motion of the digits and wrist is initiated in patients with volar plate fixation with good bone stock and solid fixation. In patients with soft osteopenic bone, digital range of motion exercises are initiated immediately, but wrist range of motion is delayed approximately 3 to 4 weeks to permit some fracture healing. Soft bone may collapse around the rigid plate. Patients treated with percutaneous K-wires have their wrist immobilized until the wires are removed, which usually happens 4 to 6 weeks after surgery. A patient with an unstable DRUJ treated by TFCC repair or ulnar styloid reduction and fixation is restricted from pronation and supination for 2 to 4 weeks.
OUTCOMES
Arthroscopically assisted fixation of displaced intra-articular distal radius fractures has shown promising results. It has been observed to provide increased range of motion, and patients with arthroscopically assisted fixation have shown better results and improved range of motion. It also aids in determining when to fix the ulnar styloid.
COMPLICATIONS
Complications of arthroscopically assisted reduction of distal radius fractures include failure of fixation, flexor and extensor tendon irritation, painful metal requiring removal, neuromas of the dorsal sensory branch of the radial and ulnar nerves, carpal tunnel syndrome, reflex sympathetic dystrophy, and wrist and hand stiffness.
- Following anatomic reduction of the distal radius fracture, insert the arthroscope in the dorsal 3/4 portal and the probe in the 6R portal. Palpate the tension of the articular disc.
- Good tension indicates that the majority of the peripheral TFCC fibers are intact or still attached to the proximal ulna.
- A peripheral tear of the articular disc is repaired arthroscopically when detected.
- Stabilization of a large ulnar styloid fragment is considered when the articular disc is lax by palpation and no peripheral TFCC is identified (TECH FIG 5).
- In this instance, the majority of the fibers of the TFCC are attached to the displaced ulnar styloid fragment.
- Make a small incision between the extensor carpi ulnaris and the flexor carpi ulnaris tendons and identify the fracture site.
- Retrieve the distal fragment, which often displaces in a distal and radial direction.
- Mobilize the styloid fragment using a no. 15 blade, taking care to protect the TFCC insertion.
- Reduce the fragment anatomically, under direct visualization, and insert a guidewire in a retrograde manner for provisional stability.
- Stabilize the ulnar styloid fragment using either a tension band technique (with wire and two K-wires) or, preferably, using a micro headless cannulated screw.
- Place the cannulated headless screw over the guidewire and verify fracture reduction with fluoroscopy.
- Insert the arthroscope into the 3/4 portal and the probe into the 6R portal to document restoration of TFCC tension.G 5.
- In this case, following reduction to the distal radius fracture, the articular disc was palpated and found to be lax but with no peripheral tear. The large ulnar styloid fragment was reduced with a micro Acutrak screw (Acumed, Hillsboro, OR).
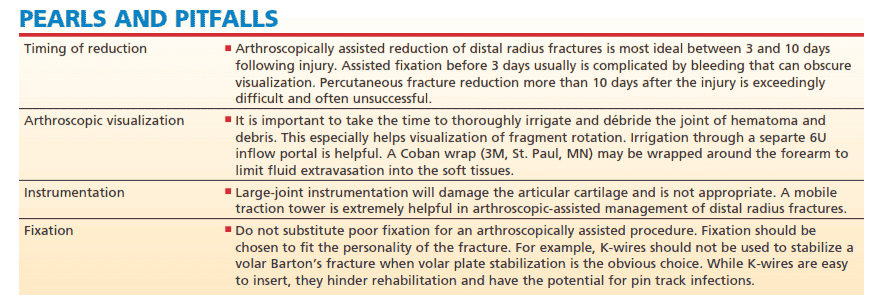
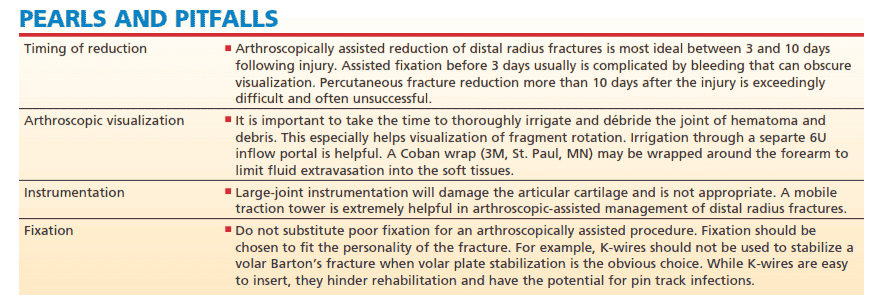
PEARLS AND PITFALLS
- Timing of reduction: Arthroscopically assisted reduction of distal radius fractures is most ideal between 3 and 10 days following injury.
- Assisted fixation before 3 days usually is complicated by bleeding that can obscure visualization.
- Percutaneous fracture reduction more than 10 days after the injury is exceedingly difficult and often unsuccessful.
- Arthroscopic evaluation: It is important to take the time to thoroughly irrigate and débride the joint of hematoma and debris.
- Large-joint instrumentation will damage the articular cartilage and is not appropriate.
- Fixation should be chosen to fit the personality of the fracture.
- Cannulated screws are recommended when arthroscopically stabilizing a fracture of the distal radius without metaphyseal comminution.
- Volar plate fixation is recommended when metaphyseal comminution is present.
- It is imperative following arthroscopically assisted reduction of the distal radius in the radiocarpal space to evaluate the midcarpal space.
OUTCOMES AND COMPLICATIONS
The literature is relatively sparse regarding the results of arthroscopically assisted fixation of displaced intra-articular distal radius fractures.
Complications may include, but are not limited to: failure of fixation, late settling of the fracture despite fixation, flexor and extensor tendon irritation, painful metal requiring removal, neuromas of the dorsal sensory branch of the radial and ulnar nerves, carpal tunnel syndrome, reflex sympathetic dystrophy, and wrist and hand stiffness.
>
In this section on arthroscopic-assisted reduction of distal radius fractures, it is important to follow the proper techniques and timing for optimal outcomes. Arthroscopically assisted reduction should ideally be done between 3 and 10 days after injury, as fixation before 3 days can be complicated by bleeding and percutaneous reduction more than 10 days after the injury is often unsuccessful. Thorough irrigation and débridement of the joint are important for good visualization, and instrumentation should be carefully chosen to avoid damaging the articular cartilage. Proper fixation should be chosen to fit the fracture type, such as volar plate stabilization for volar Barton's fractures rather than K-wires, which can hinder rehabilitation and cause pin track infections. Cannulated screws are recommended for stabilizing distal radius fractures without metaphyseal comminution, while volar plate fixation is recommended for fractures with metaphyseal comminution. Arthroscopic evaluation during screw placement is helpful for ensuring stability and avoiding joint violation. After arthroscopically assisted reduction in the radiocarpal space, it is important to evaluate the midcarpal space for intercarpal stability and to check for loose bodies. Arthroscopic evaluation can also aid in determining when to fix the ulnar styloid.
REFERENCES
1. Bradway JK, Amadio PC, Cooney WP. Open reduction and internal fixation of displaced comminuted intraarticular fractures of the distal end of the radius. J Bone Joint Surg Am 1989;71A:839–847.
2. Doi K, Hatturi T, Otsuka K, et al. Intraarticular fractures of the distal aspect of the radius arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am 1999;81A:1093–1110.
3. Edwards CC III, Harasztic J, McGillivary GR, et al. Intraarticular distal radius fractures: arthroscopic assessment of radiographically assisted reduction. J Hand Surg Am 2001;26A:1036–1041.
4. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg Am 1991;16:375–384.
5. Geissler WB. Arthroscopically assisted reduction of intra-articular fractures of the distal radius. Hand Clin 1995;11:19–29.
6. Geissler WB. Intra-articular distal radius fractures: the role of arthroscopy? Hand Clin 2005;21:407–416.
7. Geissler WB, Freeland AE. Arthroscopically assisted reduction of intra-articular distal radial fractures. Clin Orthop Relat Res 1996;327:125–134.
8. Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am 1996;78A:357–365.
9. Geissler WB, Savoie FH. Arthroscopic techniques of the wrist. Mediguide to Orthopedics 1992;11:1–8.
10. Hanker GJ. Wrist arthroscopy in distal radius fractures. Proceedings of the Arthroscopy Association North America Annual Meeting, Albuquerque, NM, October 7–9, 1993.
11. Hixon ML, Fitzrandolph R, McAndrew M, et al. Acute ligamentous tears of the wrist associated with Colles fractures. Proceedings of the Annual Meeting of the American Society for Surgery of the Hand, Baltimore, 1989.
12. Hollingworth R, Morris J. The importance of the ulnar side of the wrist in fractures of the distal end of the radius. Injury 1976;7:263.
13. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am 1986;68A:647–658.
14. Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury 1989;20:208–210.
15. Levy HJ, Glickel SZ. Arthroscopic assisted internal fixation of intraarticular wrist fractures. Arthroscopy 1993;9:122–123.
16. Lindau T. Treatment of injuries to the ulnar side of the wrist occurring with distal radial fractures. Hand Clin 2005;21:417–425.
17. Melone CP. Articular fractures of the distal radius. Orthop Clin North Am 1984;15:217–235.
18. Mohanti RC, Kar N. Study of triangular fibrocartilage of the wrist joint in Colles fracture. Injury 1979;11:311–324.
19. Mudgal CS, Jones WA. Scapholunate diastasis: a component of fractures of the distal radius. J Hand Surg Br 1990;15:503–505.
20. Ruch DS, Vallee J, Poehling GG, et al. Arthroscopic reduction versus fluoroscopic reduction in the management of intra-articular distal radius fractures. Arthroscopy 2004;20:225–230.
21. Short WH, Palmer AK, Werner FW, et al. A biomechanical study of distal radial fractures. J Hand Surg Am 1987;12:529–534.
22. Stewart NJ, Berger RA. Comparison study of arthroscopic as open reduction of comminuted distal radius fractures. Abstract. Presented at the 53rd Annual Meeting of the American Society for Surgery of the Hand. January 11, 1998, Scottsdale, AZ.
23. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am 1994;19:325–340.