Scapula Fractures
Scapula Fractures overview.
Summary
Scapula Fractures are uncommon fractures to the shoulder girdle caused by high energy trauma and associated with pulmonary injury, head injury, and increased injury severity scores.
Diagnosis can be made with plain radiographs and CT studies are helpful for fracture characterization and surgical planning.
Treatment is usually nonoperative with a sling. Surgical management is indicated for intra-articular fractures, displaced scapular body/neck fractures, open fractures, and those associated with glenohumeral instability.
Epidemiology
Incidence
rare
<1% of all fractures
3-5% of shoulder girdle fractures
Demographics
age
commonly between 25-50
males > females
Location 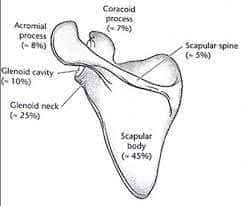
scapular body/spine = 45-50%
glenoid = 35%
glenoid neck = 25%
glenoid fossa/rim = 10%
often associated with impaction of humeral head into glenoid
acromion = 8%
coracoid = 7%
Etiology
Pathophysiology
mechanism of injury
high-energy trauma (80-90%)
motor vehicle collisions
account for >70% of scapula fractures
indirect trauma through fall on outstretched hand
glenohumeral dislocation
anterior dislocation leads to anterior rim fracture
posterior dislocation leads to posterior rim fracture
seizure
electric shock
Associated injuries (in 80-95%)
medical
orthopedic 
Anatomy
Osteology
scapular body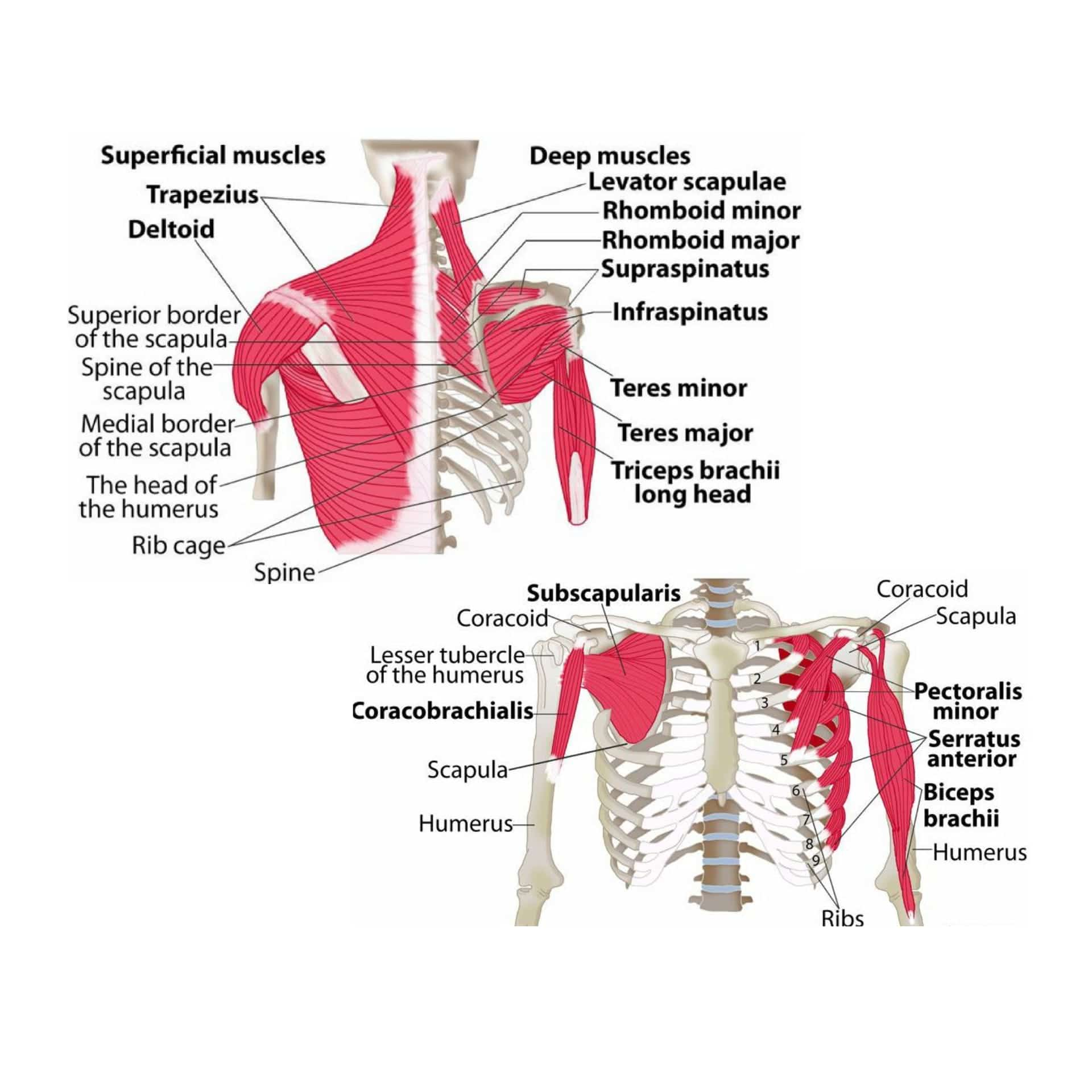
origin or insertion of 18 muscles
function to connect scapula to thorax, spine and upper extremity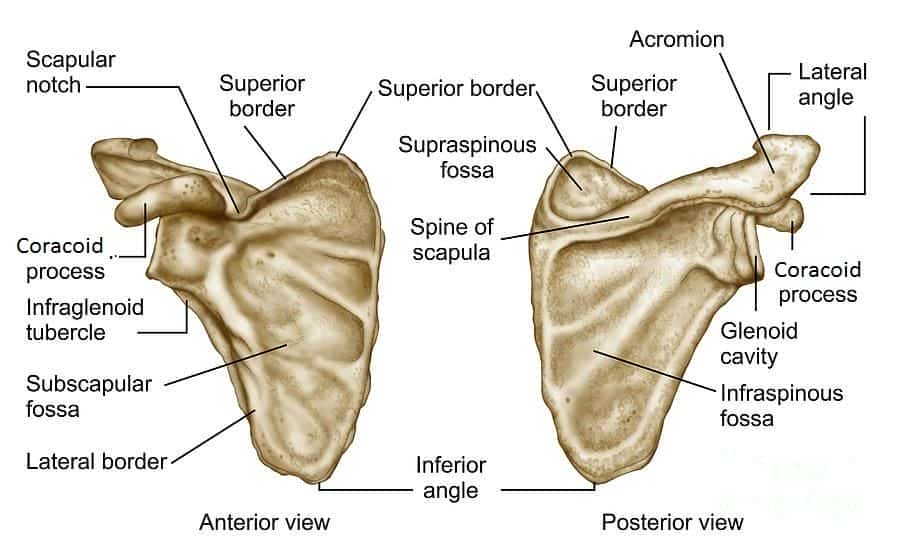
large triangle shape with 4 major processes
scapular spine
osseous bridge separating supraspinatus and infraspinatus
spinoglenoid notch represents possible site of compression for suprascapular nerve
glenoid
represents articulating process on lateral scapula serving as socket for glenohumeral joint
pear-shaped and wider inferiorly from anterior to posterior
average 1-5º of retroversion and 15º superior tilt from scapular plane
fibrocartilaginous labrum deepens glenoid fossa by 50% to increase stability
acromion
articulates with clavicle to form acromioclavicular joint
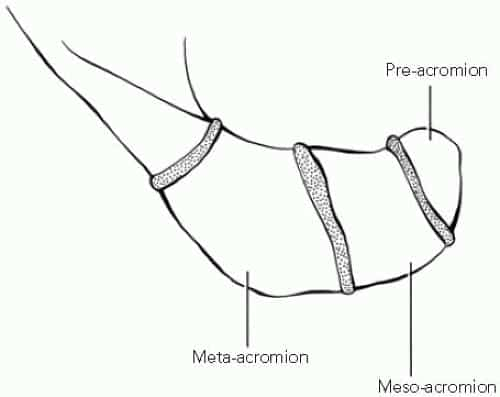 formed by 3 ossification centers
formed by 3 ossification centers
pre acromion - tip
meso acromion - mid
meta acromion - base
coracoid process
has two secondary ossification centers that are open until around age 25 and should not be interpreted as fracture
angle of coracoid
tip of coracoid
muscular attachments
conjoint tendon
coracobrachialis
short head biceps
pectoralis minor
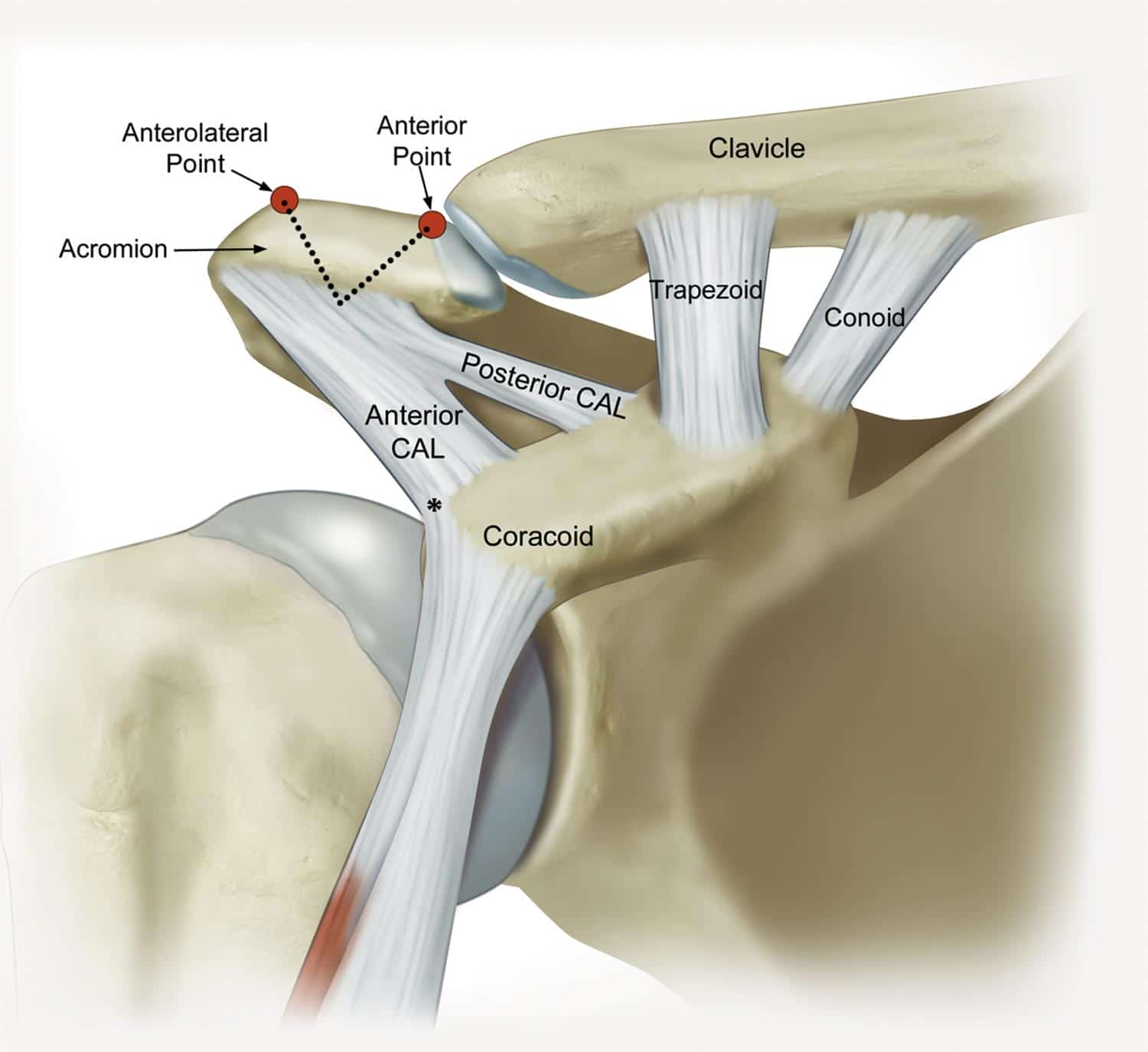
ligament attachments
coracoclavicular (CC) ligaments
most anterior CC ligament attachment is 25mm from tip of coracoid
coracoacromial ligament
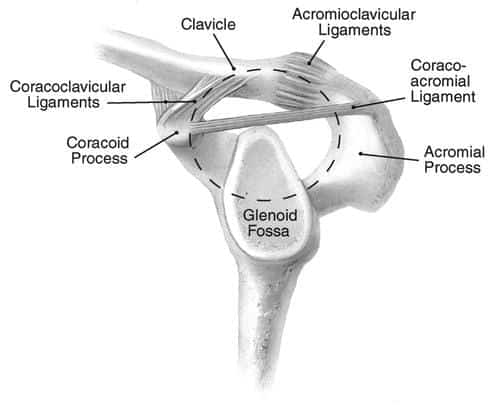
Arthrology
glenohumeral joint
glenoid & labrum support humeral head to produce high degree of motion
stability provided by static and dynamic stabilizers
scapulothoracic joint
not a true joint but does represent an articulation between scapula and thorax
involved primarily in elevation and depression of shoulder as well as rotation and pro-/retraction
acromioclavicular (AC) joint
articulation of acromion and distal clavicle
supported by acromioclavicular ligaments (horizontal stability) and coracoclavicular ligaments (vertical stability)
8º of rotation occurs through acromioclavicular joint
superior shoulder suspensory complex
bone & soft tissue ring which provides connection of glenoid/scapula to axial skeleton
composed of 4 bony landmarks
distal clavicle
acromion
coracoid
glenoid
also composed of ligamentous complexes of acromioclavicular and coracoclavicular joints
Blood supply
contributions from anterior and posterior circumflex, scapular circumflex and suprascapular arteries
watershed area present in anterosuperior glenoid
Nervous system
scapula is intimately associated with brachial plexus
axillary nerve is at risk inferior to the glenoid as it runs from anterior to posterior
compression of suprascapular nerve at scapular notch leads to supraspinatus/infraspinatus weakness, with compression at the spinoglenoid notch leading only to infraspinatus weakness
Biomechanics
scapula contributes to glenohumeral rotation and abduction
1/3 of shoulder motion is scapulothoracic, 2/3 is glenohumeral
Classification
-
Classification is based on the location of the fracture and includes
-
scapular body fractures
-
usually described based on anatomic location
-
-
scapular neck fractures
-
look for associated AC joint separation or clavicle fracture
-
if occuring together, known as "floating shoulder"
-
-
-
glenoid fractures
-
Ideberg classification with Goss modification (below)
-
low inter- and intra-observer reliability and questionable association with management
-
-
AO-OTA classification
-
more reliable in diagnosis than Ideberg classification
-
-
-
acromial fractures
-
Kuhn classification
-
-
coracoid fractures
-
Ogawa classification - based on fracture proximity to CC ligaments
-
Eyres classification
-
-
scapulothoracic dissociation
-
-
-
Presentation
-
History
-
traumatic direct blow to shoulder or fall on outstretched arm
-
scapula fracture may be missed or diagnosed late in presence of other distracting, traumatic injuries
-
Symptoms
-
diffuse, severe shoulder pain
-
systemic symptoms
-
shortness of breath
-
chest wall pain
-
Physical exam
-
inspection
-
tenderness to palpation
-
shoulder diffusely
-
inaccurate in determining specific location of fracture
-
clavicle
-
spine
-
rib cage
-
evaluate for abnormal shoulder contour compared to contralateral site
-
look for open wounds or abrasions
-
soft tissue swelling may be significant
-
motion
-
acute active range of motion testing not recommended
-
likely to cause unnecessary pain
-
gentle passive range of motion can be useful in noting any blocks to motion
-
neurovascular
-
check motor and sensory function of nerves at risk
-
axillary
-
radial
-
median
-
ulnar
-
confirm symmetry of extremity pulses to contralateral side
-
Imaging
-
Radiographs
-
recommended views
-
true AP, grashey AP, scapular Y and axillary lateral view
-
AP chest radiograph
-
evaluate for pneumothorax
-
evaluate for widening of space between medial scapular border and spine