Dorsal Approach to the Wrist
The dorsal approach provides excellent exposure of all the extensor tendons that pass over the dorsal surface of the wrist. It also allows access to the dorsal aspect of the wrist itself, the dorsal aspect of the carpus, and the dorsal surface of the proximal ends of the middle metacarpals. Its uses include the following:
1. Synovectomy and repair of the extensor tendons in cases of rheumatoid arthritis; dorsal stabilization of the wrist1,2
2. Wrist fusion3
3. Excision of the lower end of the radius for benign or malignant tumors
4. Open reduction and internal fixation of certain distal radial and carpal fractures and dislocations, including dorsal metacarpal dislocations, displaced intra-articular dorsal lip fractures of the radius, and transscaphoid perilunate dislocations. A variety of approaches are possible depending on the anatomy of the fracture to be treated. Access to the intermediate and radial columns of the distal radius will be described. Plates applied to the dorsal surface of the distal radius frequently cause irritation to the numerous extensor tendons that pass over their surface.4 For this reason, volar approaches are now often preferred for plate fixation of fractures of the distal radius.5
5. Proximal row carpectomy6,7
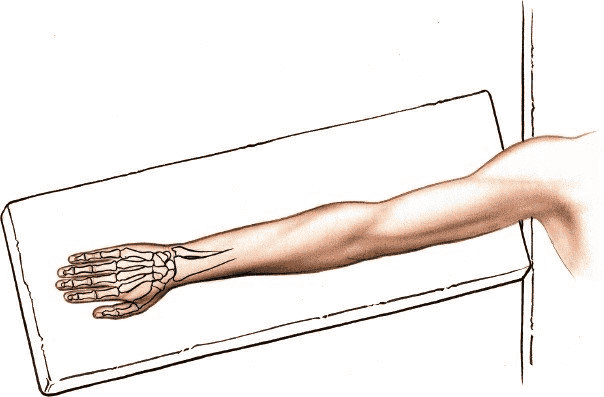
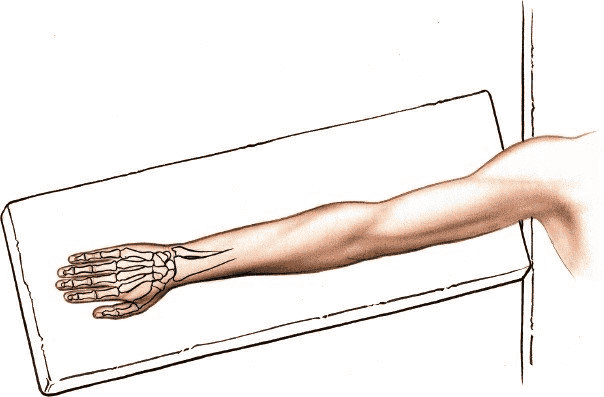
Position of the Patient
Place the patient supine on the operating table. Pronate the forearm and put the arm on an arm board. Exsanguinate the limb by applying a soft rubber bandage, and then inflate a tourniquet (Fig. 5-1).
Landmarks and Incision
Landmarks
Palpate the radial styloid, the most distal extension of the lateral side of the radius.
Palpate the ulnar styloid on the dorsal aspect of the distal end of the ulna.
Incision
Make an 8-cm longitudinal incision on the dorsal aspect of the wrist, crossing the wrist joint midway between the radial and ulnar styloids. Begin the incision 3 cm proximal to the wrist joint and end about 5 cm distal to it. It can be lengthened if necessary (Fig. 5-2).
Because the skin on the dorsum of the wrist is pliable and redundant, the healed incision does not cause a contracture of the wrist joint, even though it crosses a major skin crease at right angles.
Internervous Plane
There is no true internervous plane because the extensor muscles whose tendons are separated share a common nerve supply from the posterior interosseous nerve. Because these muscles receive their nerve supply at the level of the elbow or just below it the intermuscular plane between them can be used safely.
Superficial Surgical Dissection
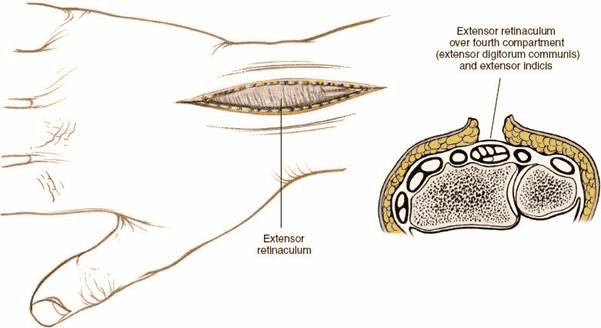
Incise the subcutaneous fat in line with the skin incision to expose the
extensor retinaculum that covers the tendons in the six compartments on the dorsal aspect of the wrist (Fig. 5-3).
Deep Surgical Dissection
The deep dissection depends on the procedure to be performed. Four techniques will be described.
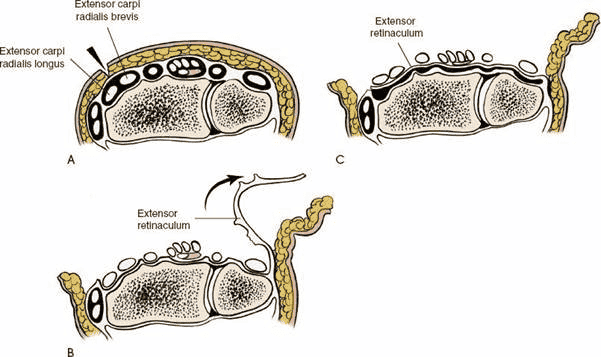
Synovectomy
Incise the extensor retinaculum over the extensor carpi radialis longus and brevis muscles in the second compartment of the wrist. The compartment is on the radial side of Lister tubercle. To expose the other compartments, incise the ulnar edge of the cut retinaculum by sharp dissection in an ulnar direction to deroof sequentially the four compartments on the ulnar side. Then, dissect the radial edge of the cut extensor retinaculum radially to deroof the first compartment. The extensor retinaculum should be preserved; during closure, it can be sutured underneath the extensor tendons to prevent them from being abraded by the bones, which can be deformed grossly by rheumatoid arthritis (Fig. 5-4).
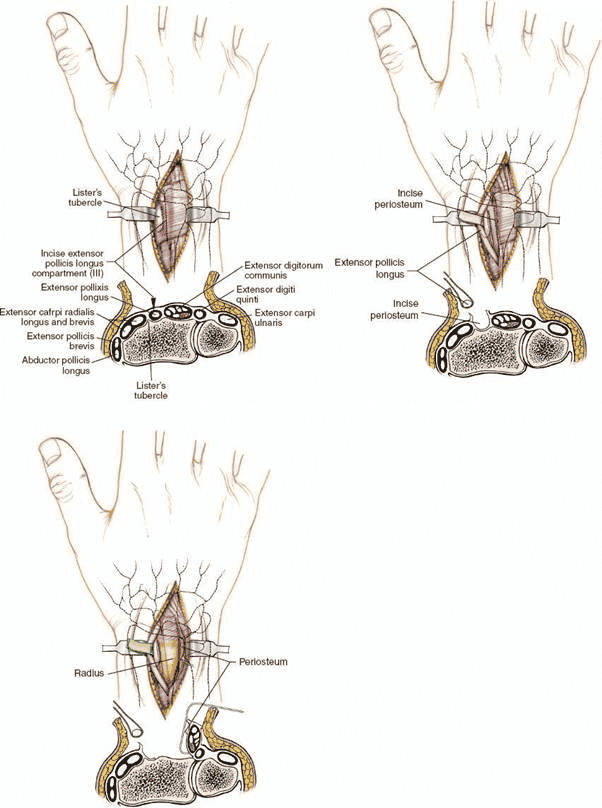
Exposure of the Intermediate Column of the Distal Radius
Identify the tendon of the extensor pollicis longus by palpation using Lister tubercle as a guide. Incise the extensor retinaculum using an angled incision overlying the tendon to open the third extensor compartment. Gently mobilize the tendon of extensor pollicis longus and retract it radially using a vascular loop. Elevate the fourth compartment subperiosteally leaving the compartment itself intact. The intermediate column of the distal radius is now exposed. If access to the joint is required make a small transverse incision into the wrist joint capsule. Suturing the retinacular incision underneath the tendon of extensor pollicis longus will protect the tendon from abrasion between the tendon and underlying plate (Fig. 5-5).
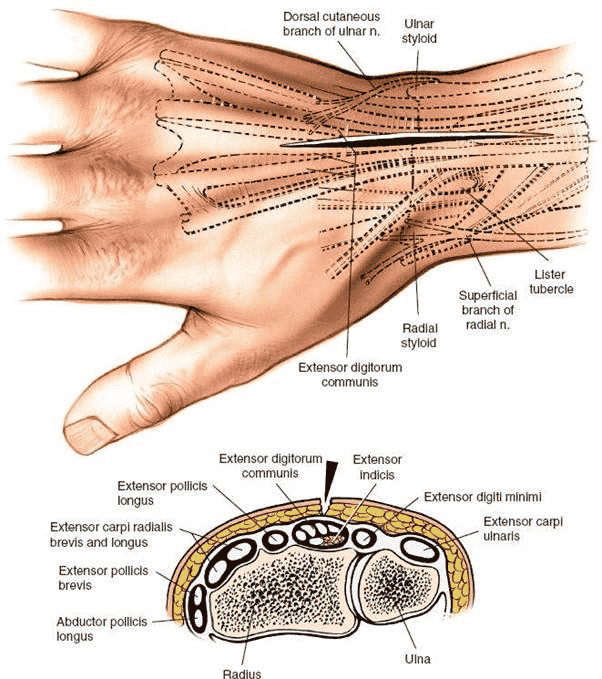
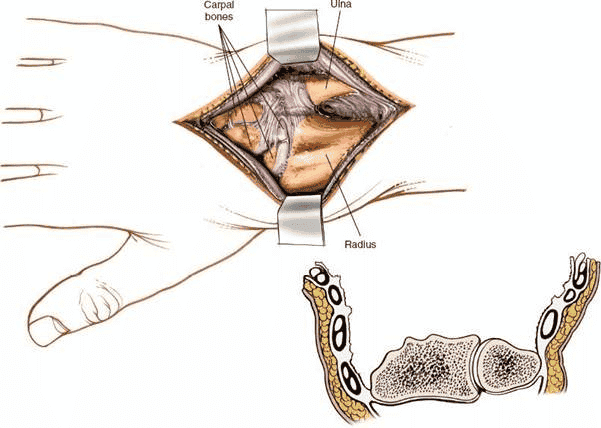
Figure 5-2 Skin incision for the dorsal approach to the wrist joint. A cross section at the distal portion of the radius is seen.
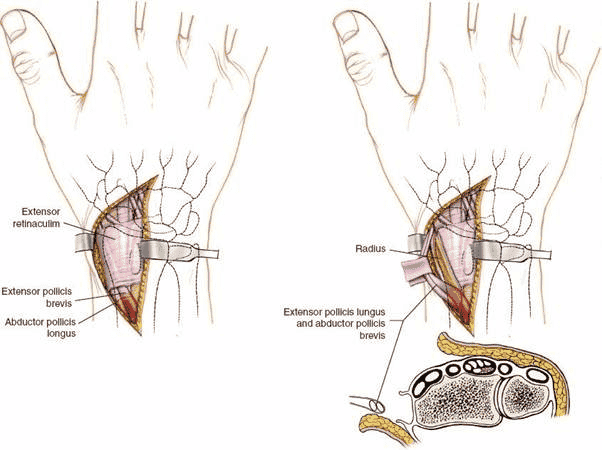
Exposure of the Radial Column of the Distal Radius
Gently retract the radial side skin flap to expose the extensor retinaculum covering the first compartment. Palpate the tendons of extensor pollicis brevis and abductor pollicis longus and incise the retinaculum at the musculotendinous junction of these two muscles. Retract the two tendons radially to expose the radial column of the distal radius (Fig. 5-6).
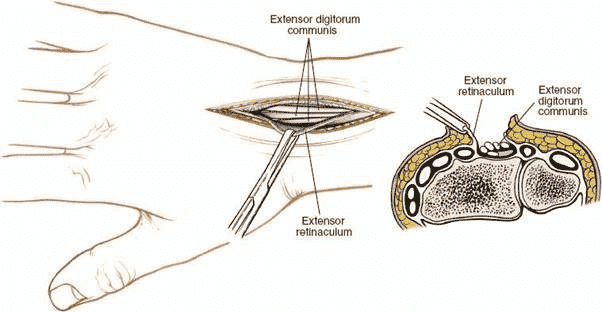
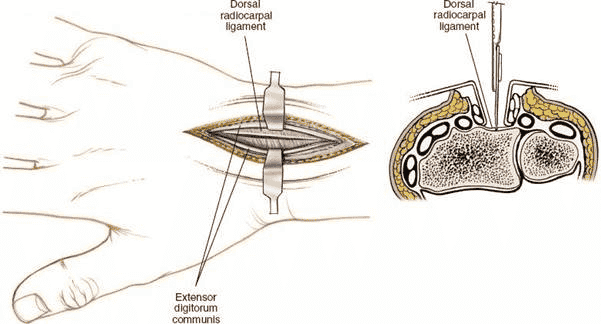
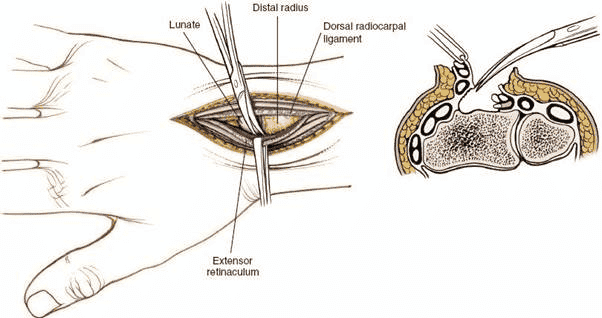
Full Exposure of the Wrist Joint
This exposure is usually used for arthrodesis of the wrist joint and is not used for fracture reduction and fixation. Incise the extensor retinaculum over the extensor digitorum communis and extensor indicis proprius tendons in the fourth compartment of the wrist. Mobilize the tendons of the compartment, lifting them from their bed in an ulnar and radial direction to expose the underlying radius and joint capsule (Fig. 5-7). Incise the joint capsule longitudinally on the dorsal aspect of the radius and carpus (Fig. 5-8). Continue the dissection below the capsule (the dorsal radiocarpal ligament) toward the radial and ulnar sides of the radius to expose the entire distal end of the radius and carpal bones (Figs. 5-9 and
5-10).
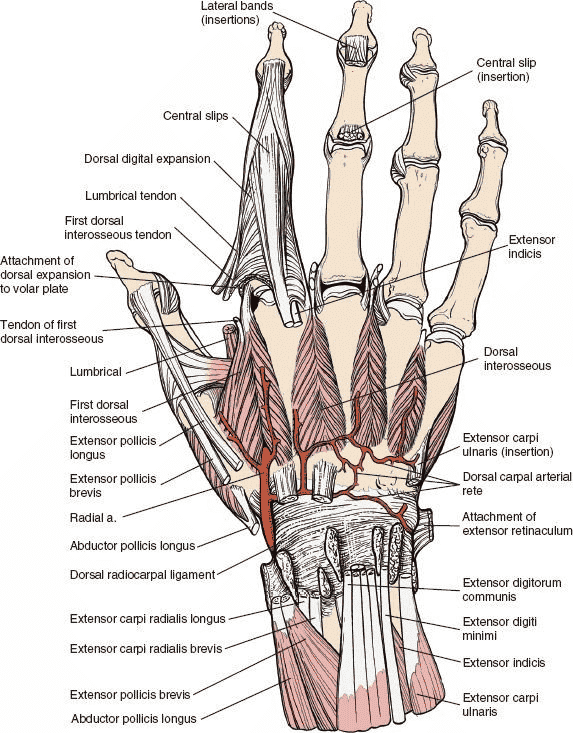
The tendons of the extensor carpi radialis longus and brevis muscles, which attach to the bases of the second and third metacarpals and lie in a tunnel on the radial side of Lister tubercle, must be retracted radially to expose fully the dorsal aspect of the carpus.
Figure 5-3 Skin flaps are developed, and the extensor retinaculum is visualized in the deeper portion of the wound. Cross section reveals the approach to the fourth tunnel, which contains the extensor digitorum communis and the extensor indicis proprius.
Figure 5-4 A: For synovectomy, make an incision over the second compartment. B: Open each of the compartments sequentially from radius to ulna by incising the septum that connects the retinaculum to the carpus itself and the joint capsule. C: Now that the compartments have been deroofed, place the retinaculum between the extensor tendons and the distal ends of the radius and ulna to provide added protection for the tendons.
Figure 5-5 Enter the wrist joint by making a small transverse incision in the wrist joint capsule. The intermediate column of the distal radius and the lunate are exposed.
Figure 5-6 Retract the tendons of extensor pollicis brevis and abductor pollicislongus radially to expose the radial column of the distal radius.
Figure 5-7 The retinaculum over the fourth compartment has been opened, revealing the communis tendons.
Figure 5-8 The extensor communis tendons and extensor indicis proprius have been retracted, revealing the dorsal radiocarpal ligament and the joint capsule,which then is incised.
Figure 5-9 The dorsal radiocarpal ligament and the extensor tendons are elevated from the posterior aspect of the radius to expose the entire dorsal end of the bone.
Figure 5-10 The extensor tendons in their compartments have been elevated to expose the distal end of the radius and ulna.
Danger
Nerves
The radial nerve (superficial radial nerve) emerges from beneath the tendon of the brachioradialis muscle just above the wrist joint before traveling to the dorsum of the hand. The skin incision lies between skin that is supplied by cutaneous branches of the ulnar nerve and skin that is supplied by cutaneous branches of the radial nerve. Damage to cutaneous nerves commonly occurs if the dissection of the flaps is begun within the fat layer. If the skin incision is taken down to the extensor retinaculum before the ulnar and radial flaps are elevated, the nerves are protected by the full thickness of the fat. Take care, however, to identify and preserve any nerve branches that are encountered during the incision of the subcutaneous tissue (Fig. 5-11). The area overlying the second extensor compartment is the commonest site for the nerve to be found.
Cutting a cutaneous nerve may result in a painful neuroma, but the resultant sensory defect rarely is significant.
Vessels
The radial artery crosses the wrist joint on its lateral aspect. As long as the dissection at the level of the wrist joint remains below the periosteum, the artery is difficult to damage.
How to Enlarge the Approach
Because it does not make use of an internervous plane, the incision cannot be extended proximally to expose the rest of the radius. It can be extended to expose the distal half of the dorsal aspect of the radius, however, by retracting the abductor pollicis longus and extensor pollicis brevis muscles, which cross the operative field obliquely.
To expose the entire dorsal surface of the metacarpals, extend the incision distally and retract the extensor tendons. (This type of extension seldom is required in practice.) The approach provides excellent exposure of the wrist joint and allows easy access to all six compartments of the extensor tunnel.
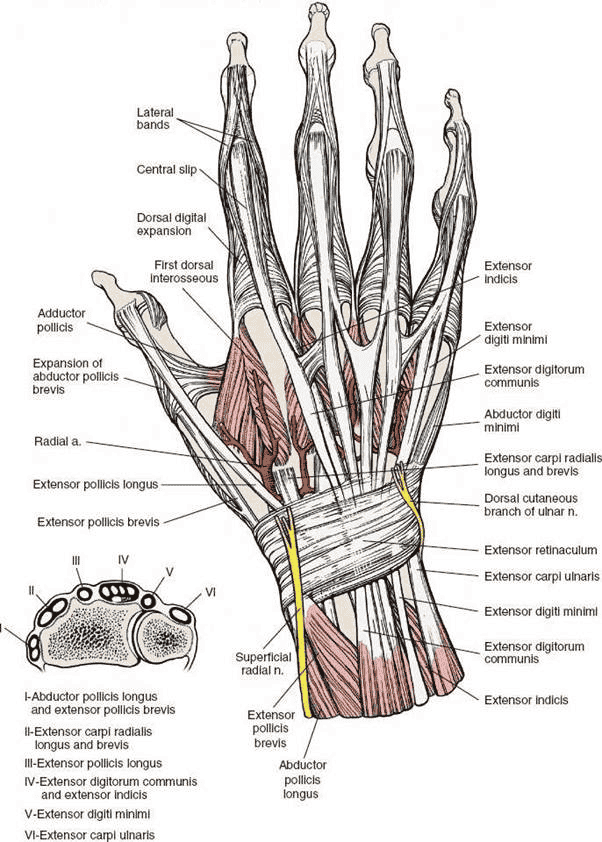
Figure 5-11 The dorsal aspect of the wrist and hand. Cross section of the distal forearm (inset). Note the compartmentalization of tendons into six distinct tunnels at the dorsal aspect of the distal forearm.
Applied Surgical Anatomy of the Dorsal Approach to the Wrist
Overview
Twelve tendons cross the dorsal aspect of the wrist joint and pass beneath the extensor retinaculum, which is a thickening of the deep fascia of the forearm. The extensor retinaculum prevents the tendons from “bowstringing.” Fibrous septa pass from the deep surface of the retinaculum to the bones of the forearm, dividing the extensor tunnel into six compartments. These septa must be separated from the retinaculum so that each compartment can be opened in surgery (see Fig. 5-11).
Landmarks and Incision
Landmarks
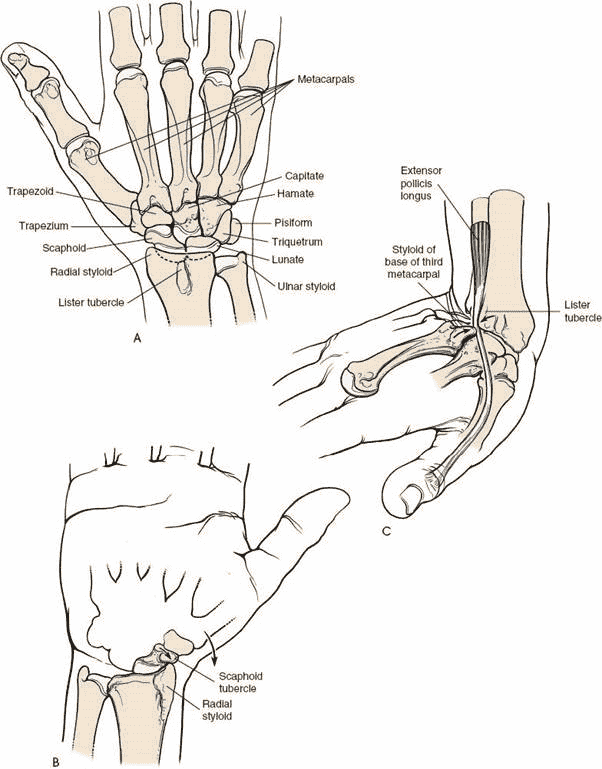
Two bony landmarks lie on the dorsal aspect of the wrist. The styloid process is the distal end of the lateral side of the radius. It also is the site of attachment of the tendon of the brachioradialis muscle. Its medial part articulates with the scaphoid bone (see Fig. 5-14A). Strong and sudden radial deviation of the wrist may cause the radial styloid process to slam into the scaphoid and fracture it (see Fig. 5-14B). Alternatively, such a force may cause a fracture of the radial styloid.
The styloid process often is excised when the scaphoid fails to unite or after arthritic changes in the wrist joint have affected the radial margin of the radioscaphoid joint. This procedure may be carried out in conjunction with a scaphocapitolunate arthrodesis.8
Lister tubercle (the dorsoradial tubercle) is a small bony prominence on the dorsum of the radius. The tendon of the extensor pollicis longus muscle angles around its distal end, changing direction about 45 degrees as it does so. When the wrist is hyperextended, the base of the third metacarpal comes very close to Lister tubercle, and the two bones can crush the trapped tendon of the extensor pollicis longus. This probably is the reason the tendon suffers delayed rupture in some cases of minimal or undisplaced fractures of the distal radius; the tendon sustains a vascular insult at the time of the original injury, even though it remains intact (see Fig. 5-14C).6
Incision
Longitudinal incisions crossing the lines of cleavage of the skin almost perpendicularly on the dorsum of the wrist can cause broad scarring. Nevertheless, because the skin on the wrist is so loose, this is one of those rare occasions when a skin incision can cross a major skin crease at right angles without causing a joint contracture.
Superficial and Deep Surgical Dissection
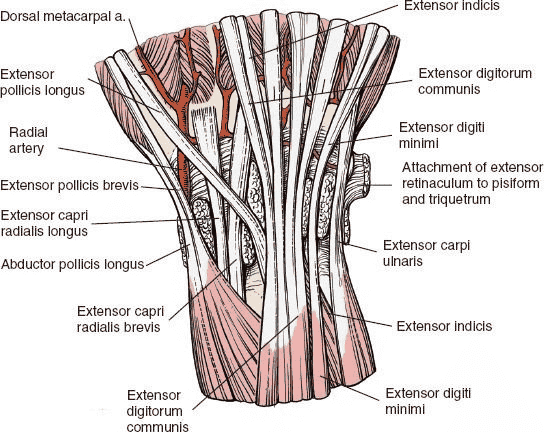
The extensor retinaculum is a narrow (2-cm) fibrous band that lies obliquely across the dorsal aspect of the wrist. Its radial side is attached to the anterolateral border of the radius; its ulnar border is attached to the pisiform and triquetral bones. (Were it attached to both bones of the forearm instead, pronation and supination would be impossible, because its fibrous tissue is incapable of stretching the necessary 30%.)
Fibrous septa pass from the deep surface of the extensor retinaculum to the bones of the carpus, dividing the extensor tunnel into six compartments (Fig. 5-12). From the radial (lateral) to the ulnar (medial) aspect, the compartments contain the following:
I. Abductor pollicis longus and extensor pollicis brevis. These tendons lie over the lateral aspect of the radius. They may become trapped or inflamed beneath the extensor retinaculum in their fibroosseous canal, producing de Quervain disease (tenosynovitis stenosans). Access to this compartment is required to apply plates to the radial column of the wrist joint.
II. Extensor carpi radialis longus and extensor carpi radialis brevis. These muscles run on the radial side of Lister tubercle before reaching the dorsum of the hand. The tendon of the extensor carpi radialis longus is used frequently in tendon transfers. The tendons run in separate synovial sheaths.
III. Extensor pollicis longus. This tendon passes into the dorsum of the hand on the ulnar side of Lister tubercle. It may rupture in association with fractures or rheumatoid arthritis. The oblique passage of this tendon on the dorsal aspect of the wrist creates significant problems for plate fixation of fractures of the distal radius. Tendon irritation and even rupture may occur due to abrasion of the tendon on the surface of the plate. Similar problems apply to a lesser degree with all the other extensor tendons.9
IV. Extensor digitorum communis and extensor indicis. The indicis tendon is used commonly in tendon transfers.
V. Extensor digiti minimi. This tendon overlies the distal radioulnar joint. VI. Extensor carpi ulnaris. This tendon passes near the base of the ulnar
Figure 5-12 Anatomy of the distal forearm, with the extensor retinaculum excised and the septa remaining. The retinaculum on the ulnar side inserts into the triquetrum and pisi form bones
.
styloid process. It is used sometimes in tendon transfers (Fig. 5-13; see
Fig. 5-12).
Figure 5-13 The extensor tendons have been removed, revealing the dorsal radiocarpal ligament. The radial artery is seen piercing the first dorsal interosseous muscle and contributing to the dorsal carpal rete. Note the hood mechanism for the index finger; contributions are made to it by the first dorsal interosseous and the first lumbrical muscles.
Figure 5-14 A: Dorsal aspect of the bones of the distal forearm, wrist, and proximal hand. B: A strong and sudden radial deviation of the wrist may cause the radial styloid process to impinge on the scaphoid tubercle and fracture it. C: With sudden extreme dorsiflexion of the wrist, as when one falls on an outstretched hand, the extensor pollicis longus tendon may be trapped or crushed between the dorsal radial tubercle (Lister tubercle) and the base of the third metacarpal.