Volar Approach to the Distal Radius
The volar approach to the distal radius provides excellent exposure of the volar aspect of the distal radius. Its use is almost exclusively in the treatment of distal radial fractures and its popularity has increased greatly in recent years since the advent of locking plates.
Other uses include the following:
1. Bone grafting for nonunions of the distal radius
2. Osteotomies of the distal radius
3. Excision of the radial styloid or release of the brachioradialis
The approach is very similar to the lower end of the anterior approach to the radial shaft but it utilizes the plane between the radial artery and the flexor carpi radialis and not the plane between the radial artery and brachioradialis. The exposure of the distal radius is therefore more ulnarward and retraction of the radial artery is not required to access the more central portions of the distal radius and wrist joint.
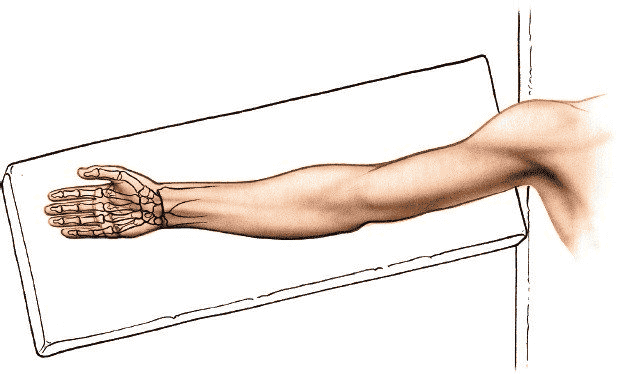
Position of the Patient
Place the patient supine on an operating table. Rest the forearm on a hand table in the supinated position so that the palm faces upward. Use an exsanguinating bandage (Fig. 5-15).
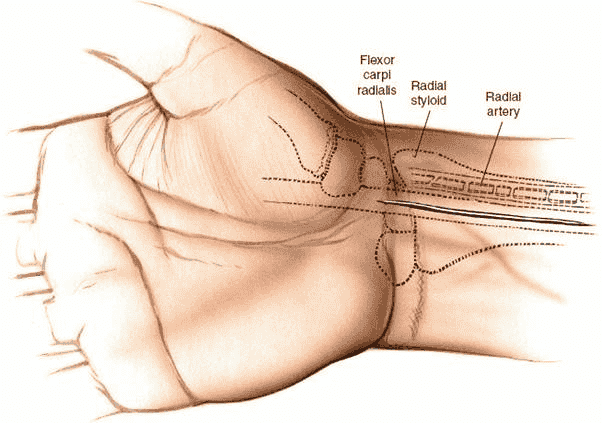
Landmarks and Incision
Landmarks
Palpate the styloid process of the radius. It is the most distal part of the lateral side of the radius. Then move in an ulna direction to palpate the tendon of flexor carpi radialis which is thick and immobile. The flexor carpi radialis muscle and tendon lie radial to the palmaris longus muscle at the level of the wrist and just to the ulnar side of the radial pulse.
Incision
Make a longitudinal incision overlying the tendon of flexor carpi radialis. Begin just above the skin crease of the wrist and extend the incision up the volar aspect of the forearm. The length of the incision will depend on the nature of the fracture pathology and the length of the plate to be used for fixation—7 cm is usually sufficient (Fig. 5-16).
Internervous Plane
The plane lies between the flexor carpi radialis supplied by the median nerve and the brachioradialis muscle supplied by the radial nerve.
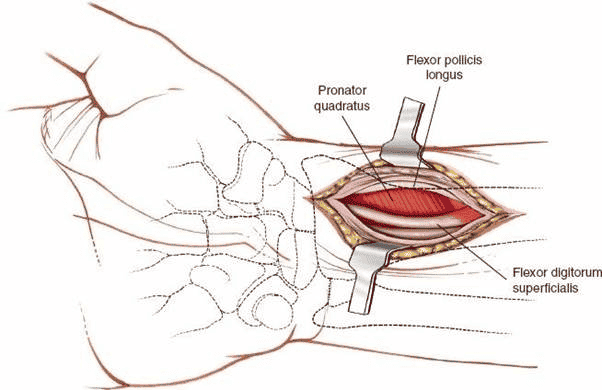
Superficial Surgical Dissection
Incise the subcutaneous fat in the line of the skin incision. Incise the deep fascia overlying the tendon of flexor carpi radialis (Fig. 5-17). Identify the radial artery radially and the tendon of flexor carpi radialis ulnarly. Develop a plane between these two structures to expose the fascia overlying the pronator quadratus muscle (Figs. 5-18 and 5-19).
Figure 5-15 Position of the patient for volar approaches to the distal radius.
Figure 5-16 Incision for volar approach to wrist. The 5- to 7-cm incision overliesthe tendon of flexor carpi radialis and ends just above the wrist joint crease.
Figure 5-17 The fascia over the tendon of flexor carpi radialis is incised and the radial artery is identified in the radial edge of the wound.
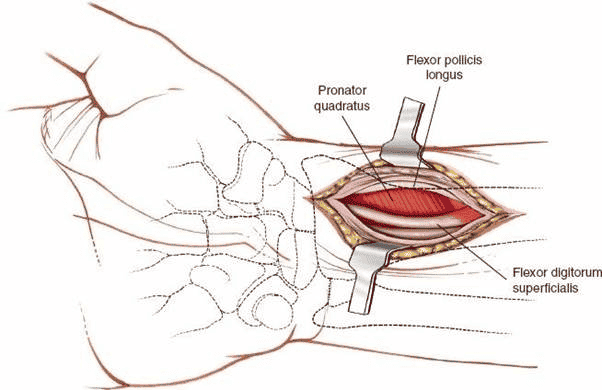
Figure 5-18 The tendon of flexor carpi radialis is retraced ulnarly to reveal the pronator quadratus muscle.
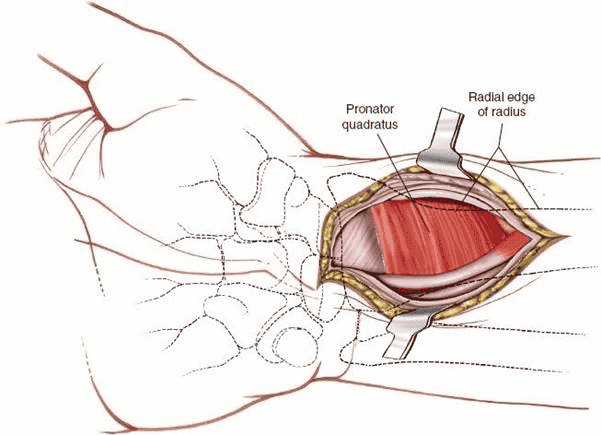
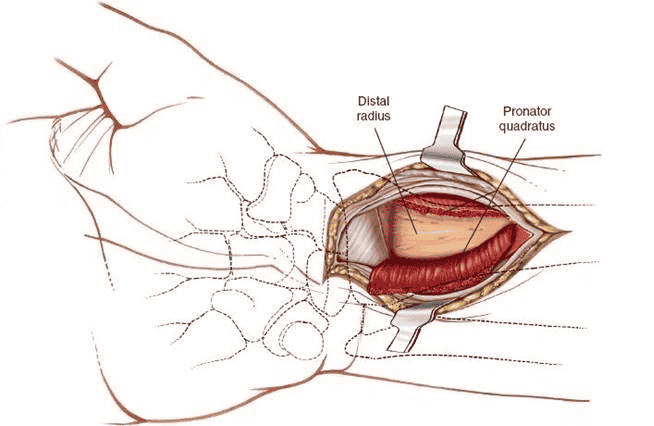
Figure 5-19 The pronator quadratus muscle is divided to expose the underlying volar aspect of the distal radius.
Figure 5-20 The pronator quadratus muscle is divided in the line of the skin incision to reveal the volar aspect of the distal radius.
Deep Surgical Dissection
The volar aspect of the distal radius is covered by the pronator quadratus muscle. Several techniques can be used to reach the bone of which three will be described. No technique has been proven to give better long-term function although minimally invasive techniques may give a slightly faster return to function.10,11
1. Complete muscle detachment
Identify the insertion of the muscle into the anterolateral border of the radius beginning just below the radial styloid process. Detach this insertion by sharp dissection. Similarly detach the insertion of the muscle to the anterior surface of the distal end of the radius raising up a triangular flap of muscle. This technique gives the opportunity to close the muscle flap after surgery protecting the more superficial flexor muscles from an anteriorly applied plate.
2. Minimally invasive technique
Identify the insertion of the muscle into the anterior surface of the distal end of the radius and detach it from the bone by sharp dissection. Leaving the lateral insertion intact tunnel underneath the muscle to expose the anterior surface of the bone. This technique is more soft tissue friendly but gives less exposure of the fracture site. Screws have to be inserted through stab incisions in the muscle.
3. Classical technique
Divide the pronator quadratus muscle in the line of the skin incision and elevate it from the anterior surface of the bone. This technique is more destructive and may be associated with slower initial recovery. Repair of the muscle is usually not possible (Fig. 5-20).
Danger
Vessels
The radial artery lies close to the lateral border of the wound and can be incised accidentally at any time during the dissection. Therefore, take care to identify and protect the artery. It is surrounded by venae comitantes and these may be easier to identify than the artery if an exsanguinating
tourniquet is used.
Nerves
The median nerve lies on the ulnar side of the approach and is protected as long as one stays radial to the flexor carpi radialis. If one strays ulnarward or do not use the pronator quadratus and its subperiosteal reflection to protect the structures on the ulnar side of the wrist, then the median nerve will be encountered and may be at risk of damage.
How to Enlarge the Approach
The incision can be extended usefully proximally and distally. Proximally, extend the skin incision along the line of the flexor carpi radialis muscle. Identify the proximal border of the pronator quadratus muscle following the internervous plane between median nerve innervated structures and radial nerve innervated structures (flexor carpi radialis and brachioradialis respectively). The exposure can also be extended distally by incising the wrist capsule and following the line of the flexor carpi radialis tendon. The tubercle of scaphoid is palpated in the distal most aspect of the incision and the wrist joint can be opened with visualization of the articular surface of the scaphoid.