Arthroscopic Reduction and Fixation of Distal Radius and Ulnar Styloid Fractures
DEFINITION
■ A bimodal age distribution exists for patients with distal radius fractures (ie, young adults vs elderly persons), and they frequently have a different mechanism of injury.
■ Patients 65 years of age or older have an annual incidence of 8 to 10 fractures of the distal radius per 1000 person-years.
■ The incidence is seven times higher in women than in men.
■ Sixteen percent of white women and 23% of white men will sustain a fracture of the distal radius after the age of
50 years.
■ Fractures of the distal radius are one of the most common skeletal injuries treated by orthopaedic surgeons.
■ These injuries account for one-sixth of all fractures that are evaluated in the Emergency Department.
■ Displaced intra-articular fractures of the distal radius are a unique subset of radius fractures.18
■ These fractures are a high-energy injury.
■ This high-energy injury results in comminuted fracture patterns.
■ These fractures are less amenable to traditional closed manipulation and casting.
■ The prognosis for these fractures depends on the amount of residual radius shortening, both radiocarpal and radioulnar articular congruity, and associated soft tissue injuries.22,24
ANATOMY
■ The distal radius serves as a plateau to support the carpus.
■ The distal radius has three concave articular surfaces: the scaphoid fossa, the lunate fossa, and the sigmoid notch.
■ The distal articular surface of the radius has a radial inclination averaging 22 degrees and palmar tilt averaging
11 degrees.
■ Radial-based volar and dorsal ligaments arise from the distal radius to support the wrist.
■ The sigmoid notch of the distal radius articulates with the ulnar head about which it rotates.
■ The distal radioulnar joint (DRUJ) is primarily stabilized by the triangular fibrocartilage complex (TFCC).
■ The sigmoid notch angles distally and medially at an average of 22 degrees.
PATHOGENESIS
■ The biomechanical characteristics of each fracture type depend on the mechanism of injury.
■ Fernandez and Geissler4 developed a classification based on
the mechanism of injury. They noted that the associated ligamentous lesions, subluxations, and associated carpal fractures are related directly to the degree of energy absorbed by the distal radius.
■ Type I fractures are bending fractures of the metaphysis in which one cortex fails to tensile stress and the opposite one undergoes a certain degree of comminution (eg, extra-articular Smith or Colles’ fractures).
■ Type II fractures are shearing fractures of the joint surface
(eg, radial styloid fractures, Barton’s fracture).
■ Type III fractures are compression fractures of the joint surface with impaction of the subcondral and metaphyseal cancellous bone (ie, intra-articular comminuted fractures).
■ Type IV fractures are avulsion fractures of ligamentous attachments, including radial styloid and ulnar styloid fractures, and are associated with radiocarpal fracturedislocations.
■ Type V fractures are high-energy injuries that involve a combination of bending, compression, shearing, and avulsion mechanisms or bone loss.
■ Several studies have shown that a high incidence of associated soft tissue injuries is seen with displaced intra-articular distal radius fractures.9,11–13,17,19,20
■ Arthroscopic studies demonstrate a high incidence of injury to the triangular fibrocartilage complex, followed by the scapholunate interosseous ligament, and then the lunotriquetral interosseous ligament (which is the least injured).
■ A spectrum of injury occurs to the interosseous ligament in which it attenuates and eventually tears and the degree of rotation between the carpal bones increases.
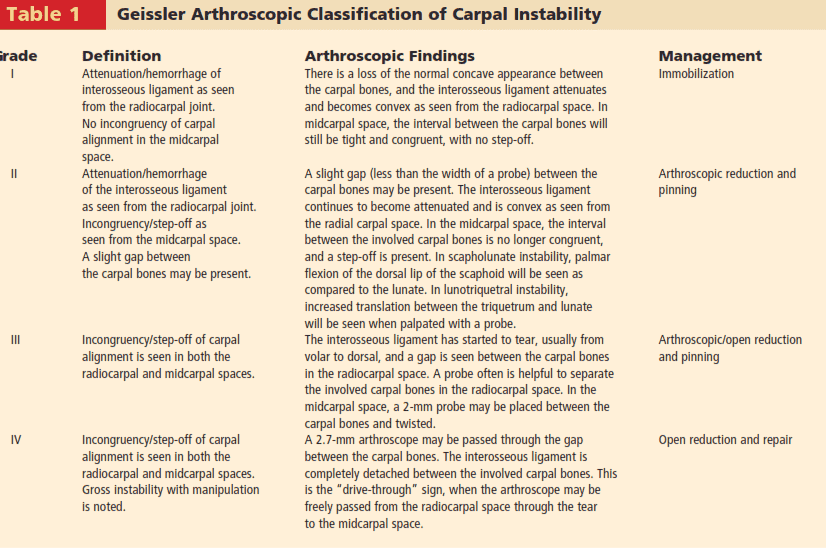
■ Geissler et al defined an arthroscopic classification of interosseous ligament tears that helps define the degree of ligament injury and secondary instability as well as proposes treatment (Table 1; see also Chap. HA-41).
NATURAL HISTORY
■ Intra-articular fractures of the distal radius have two pathologies: the associated global injury to the soft tissues and the injury to the bone itself.
■ The natural history for an intra-articular fracture of the distal radius depends on restoration of anatomy as well as detection and management of any associated soft tissue injuries.1,4
■ Knirk and Jupiter13 documented the importance of articular
restoration over extra-articular orientation in predicting outcomes for fractures of the distal radius.
■ They showed solid evidence that the largest tolerable articular step-off is 2 mm.
■ They demonstrate that the better the restoration of the articular surface, the better the outcome.
■ A loss in radius length of 2.5 mm will shift the normal load transmitted across the ulna from 20% to 42%, which may lead to various stages of ulnar impaction syndrome.
■ Untreated complete tears of the scapholunate interosseous ligament, which are highly associated with radial styloid fractures, may progress to a wrist with scapholunate advanced collapse.
PATIENT HISTORY AND PHYSICAL FINDINGS
■ A thorough history should be obtained, including the circumstances surrounding the injury as well as any additional injuries.
■ Neurologic basis
■ Cardiac basis
■ Patients’ level of independence, dominant hand, status with assisted devices, work, activity level, and support structure should be determined.
■ Physical examination, while concentrating on the wrist, should also include the hand, elbow, and shoulder to check for concomitant injuries.
■ The hand, wrist, arm, and shoulder must be carefully inspected for open injury so that tetanus and antibiotic prophylaxis may be initiated if necessary.
■ Thorough distal sensory and motor function examination should be carried out in an organized manner.
■ Vascular examination should include palpation of both the radial and ulnar pulses and determination of capillary refill time.
■ Precise palpation is used to define areas of potential trauma.
■ Diminished sensibility, pallor, altered capillary refill, increased tenseness of the soft tissues, and pain out of proportion should raise suspicion for significant soft tissue injury, including compartment syndrome.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Posteroanterior (PA), oblique, and lateral radiographs are the primary radiographic workup for distal radius fractures.
■ Contralateral radiographs of the uninvolved extremity are useful to compare radial inclination, ulnar variance, and sigmoid notch anatomy.
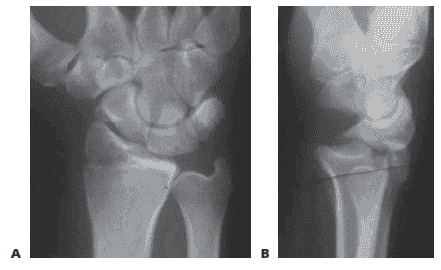
■ PA projections are useful to evaluate the radial inclination, radius height, presence of ulnar styloid fractures, widening of the DRUJ, widening of intracarpal spaces, and intra-articular involvement (FIG 1A).
■ Standard radiographic parameters of the distal radius
include radial inclination of 23 degrees (range 13–30), radius length of 12 mm (range 8–18 mm), and volar tilt of
12 degrees (range 1–21 degrees).
■ Ulnar variance shoulde be measured with the shoulder in 90 degrees of abduction, the elbow at 90 degrees of flexion, and the wrist in neutral pronation-supination.
■ A lateral projection is used to assess volar and dorsal tilt of the distal fragment, dislocation or subluxation of the DRUJ or carpus, lunate angulation, and dorsal comminution (FIG 1B).
FIG 1 • A. PA radiographic view showing a minimally displaced radial styloid fracture fragment. B. The lateral view shows a complete fracture-dislocation of the wrist.
■ A modified lateral radiograph with the beam angulating
10 to 30 degrees proximally improves visualization of the articular surface and evaluation of the volar rim of the lunate facet represented by the anterior teardrop.
■ An additional 30-degree anteroposterior (AP) cephalic projection is useful to evaluate the dorsal ulnar margin of the distal radius.
■ Oblique radiographs are very helpful, because major fracture fragments may be rotated out of their anatomic planes.
■ CT evaluation, particularly three-dimensional CT, can further delineate fragment location, joint compression, and rotation.
■ MRI evaluation is useful in assessing for associated soft tissue injuries such as TFCC tears, interosseous ligament injuries, and carpal fractures.
■ Radiographic signs that demonstrate that the distal radius fracture is likely unstable and closed reduction would be insufficient include15:
■ Lateral tilt greater than 20 degrees dorsal
■ Dorsal comminution greater than 50% of the width
■ Initial fragment displacement greater than 1 cm
■ Volar translation greater than 2 mm
■ Initial radius shortening more than 5 mm
■ Intra-articular step-off greater than 2 mm
■ Associated ulna fracture
■ Severe osteoporosis.
■ Age greater than 60 years
DIFFERENTIAL DIAGNOSIS
■ Carpal bone fracture
■ Metacarpal or phalangeal fracture
■ DRUJ disruption
■ Essex-Lopresti lesion
■ Interosseous ligament tear
■ Carpal dislocation (perilunate)
NONOPERATIVE MANAGEMENT
■ Displaced fractures of the distal radius are reduced using an adequate anesthetic agent.
■ Knowledge of the mechanisms of injury helps facilitate manual reduction. Force is applied opposite the force that caused the fracture.
■ Gentle traction is necessary to disimpact the fracture fragments, followed by palmar translation of the hand and carpus in respect to the radius.
■ The radius articular surface will rotate around the intact volar cortical lip to restore volar inclination with palmar translation.
■ Care must be taken to avoid trauma to the skin during the reduction maneuver, particularly in elderly patients where the skin may be fragile.
■ A splint is supplied following the reduction. No consensus has been established regarding wrist or forearm position, longarm versus short-arm immobilization, or splint versus cast.
■ Extreme positions of wrist flexion and ulnar deviation should be avoided.
■ Postreduction radiographs are taken in plaster.
■ Depending on stability of the fracture, most patients treated nonoperatively require weekly visits for the first 3 weeks to monitor fracture reduction.
■ In patients older than 65 years, one third of initially undisplaced fractures subsequently collapsed to some degree.
■ One study of elderly patients with moderately displaced fractures of the distal radius found that two thirds of the correction obtained by closed manipulation was lost at 5 weeks.
■ Patients with minimally displaced or nondisplaced fractures of the distal radius treated nonoperatively must be made aware of possible complications, including rupture of the extensor pollicis longus tendon, carpal tunnel syndrome, and compartment syndrome.
SURGICAL MANAGEMENT
■ Distal radius fractures without extensive metaphyseal communition are ideal candidates for arthroscopic-assisted fixation with K-wires or cannulated screws.7,8
■ Radial styloid fractures
■ Impacted fractures
■ Die punch fractures
■ Three-part T-type fractures and four-part fractures with metaphyseal comminution are best treated with a combination of volar plate stabilization. Wrist arthroscopy is used as an adjunct to fine-tune the articular reduction and evaluate for associated soft tissue lesions.
■ Distal radius fractures that may be minimally displaced, and fractures with strongly suspected associated soft tissue injury, also are candidates for arthroscopic-assisted fixation to stabilize the fracture but, more importantly, to evaluate and treat the acute associated soft tissue injury.
■ Stabilization of associated ulnar styloid fragments is controversial.13 Wrist arthroscopy provides a rationale as to when to stabilize an ulnar styloid fragment.
Preoperative Planning
■ All radiographic studies are reviewed.
■ Equipment needed for arthroscopic treatment and for open stabilization is made available.
■ Small joint instrumentation is essential for arthroscopicassisted fixation of distal radius fractures. The small joint arthroscope is approximately 2.7 mm in diameter, and even
2175
smaller scopes may be used if desired. In addition, a small joint shaver (3.5 mm or less) is useful to clear fracture debris and hematoma.
■ The ideal timing for arthroscopic-assisted fixation of distal radius fractures is 3 to 10 days following injury.6
■ Earlier attempts at fixation may be complicated by soft tissue swelling and troublesome bleeding, obscuring visualization.
■ After 10 days, the fracture fragments start to become sticky and more difficult to percutaneously elevate and reduce.
Positioning
■ Arthroscopic-assisted fixation of distal radius fractures may be performed with the arm suspended vertically in a traction tower, horizontally in a traction tower, or with finger traps applied attached to weights hanging over the edge of the hand table.
■ Wrist arthroscopy in the horizontal position may make it easier to simultaneously monitor the reduction fluoroscopically and place hardware. However, it does not allow for simultaneous volar access to the wrist.
■ Suspending the wrist in a vertical position with a traction tower allows simultaneous access to both the volar and dorsal aspects of the wrist. This is particularly useful when wrist arthroscopy is used as an adjunct to volar plate fixation of the distal radius fracture.
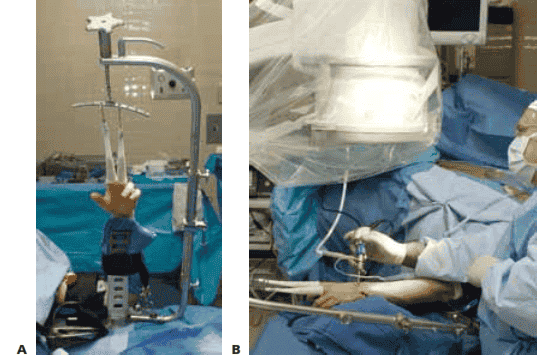
■ A new traction tower has been designed to allow simultaneous evaluatation of the intra-articular reduction of the distal radius arthroscopically and fluoroscopically (FIG 2A).
■ The surgeon may stabilize a comminuted fracture of the
distal radius with a plate and simultaneously evaluate the articular reduction arthroscopically.
■ The traction tower allows for traction of the wrist in either the vertical or horizontal planes, depending on the surgeon’s preference (FIG 2B).
Approach
■ The wrist is suspended in a traction tower, and the standard dorsal 3/4 viewing portal, 4/5 or 6R working portal, and 6U inflow portal are made.
■ It is difficult to palpate the normal extensor tendon landmarks for traditional wrist arthroscopy in patients who sustain a fracture of the distal radius because of swelling.10 However, the bony landmarks usually can still be palpated. These bony landmarks include the bases of the metacarpals, the dorsal lip of the radius, and the ulnar head.
■ The 3/4 portal is made in line with the radial border of the long finger. It is very useful to place a no. 18 needle into the proposed location of the 3/4 portal before making a skin incision.
■ If the portal is placed too proximal, the arthroscope may be placed within the fracture pattern itself. If it is placed too distal, it can injure the articular surface of the carpus.
■ Once the precise ideal location of the portal is located, the portal is made by pulling the skin with the sugeon’s thumb against the tip of a no. 11 blade. Blunt dissection is carried down with a hemostat, and the arthroscope, with a blunt trocar, is introduced into the dorsal 3/4 portal.
■ This technique decreases potential injury to cutaneous nerves.
■ Thorough irrigation of the joint is necessary to wash out fracture hematoma and debris and improve visualization. Inflow may be provided through the arthroscope cannula or separately through a no. 14 needle into the 6U portal.
■ Use of a separate 6U inflow portal is recommended. The small-joint arthroscopy cannula does not allow as much space between the cannula and the arthroscope, limiting the amount of flow through the cannula.
■ Outflow to the wrist is provided through intervenous extension tubing connected to the arthroscope cannula.
■ The 4/5 working portal is made in line with the mid-axis of the ring metacarpal. Alternatively, the 6R working portal is made just radial to the palpable extensor carpi ulnaris tendon.
■ A no. 18 needle is placed into the joint and should lie just distal to the articular disc.
■ A 4/5 or 6R portal usually is located just proximal to the
3/4 portal because of the natural radial slope of the distal radius.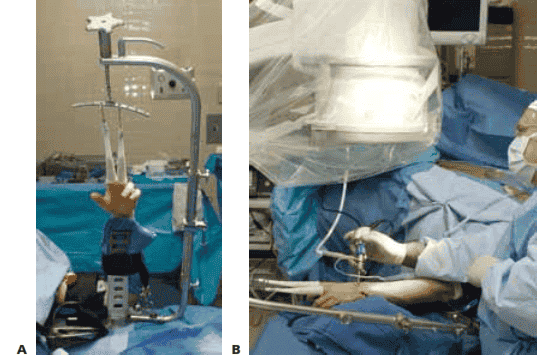
FIG 2 • A. This traction tower (Acumed, Hillsboro, OR) uses a suspension bar at the side rather than at the center of the wrist. This allows easy fluoroscopic evaluation of the fracture reduction, with simultaneous full access to the volar and dorsal aspects of the wrist. B. The tower can be flexed intoa horizontal position for surgeons who prefer to
next